More Information
Submitted: 30 October 2020 | Approved: 03 November 2020 | Published: 04 November 2020
How to cite this article: Bacha D, Guizani R, Ferjaoui W, Atallah A, Slama SB, et al. Malignant transformation of an urachal cyst. Arch Case Rep. 2020; 4: 052-053.
DOI: 10.29328/journal.acr.1001043
ORCiD: orcid.org/0000-0002-4279-9370
Copyright License: © 2020 Bacha D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Malignant transformation of an urachal cyst
Dhouha Bacha1, Rami Guizani2, Wael Ferjaoui2*, Aziz Atallah2, Sana Ben Slama1 and Ahlem Lahmar1
1Department of Pathology, Mongi Slim University Hospital, Faculty of Medicine of
Tunis, University of Tunis El Manar, Tunisia
2Department of General Surgery, Mongi Slim University Hospital, Faculty of Medicine
of Tunis, University of Tunis El Manar, Tunisia
*Address for Correspondence: Wael Ferjaoui, Department of General surgery, Mongi Slim University Hospital, Faculty of medicine of Tunis, University of Tunis El Manar, Tunisia, Tel: +216 52430099; Email: [email protected]
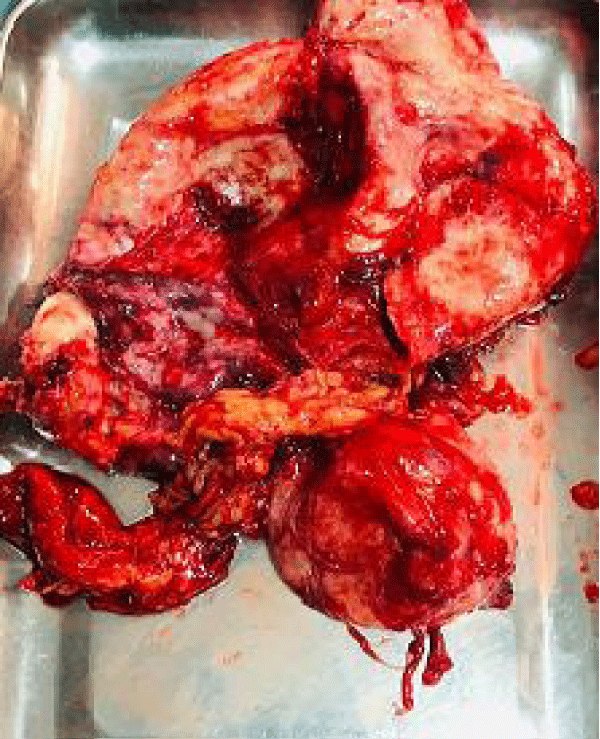
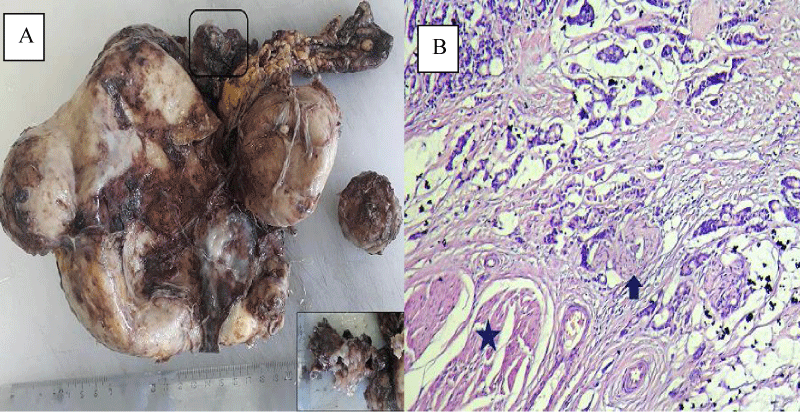
A 27-year-old man presented to our hospital for abdominal pain and a cheesy discharge from the umbilicus which lasted for a few days. He was afebrile. The physical examination revealed periumbilical tenderness and discharge from the umbilicus. There were no signs of general infection. Otherwise, he had neither specific symptoms nor a palpable abdominal mass. Pelvic computerized tomographic (CT) scanning) confirmed the presence of a cyst in the midline of the abdominal wall, with communication with the bladder and peripheral calcification. The mass was infiltrated to the perivesical fat (Figure 1). The patient was prepared for surgery. During laparotomy, a urachal cyst with the cuff of the bladder dome were removed (Figure 2). Recovery was unremarkable. The resected specimen was a partial cystectomy specimen with perivesical fat and the median umbilical ligament (Figure 3A,B).
Figure 1: Computerized tomographic (CT) scanning confirmed the presence of a cyst in the midline of the abdominal wall, with communication with the bladder and peripheral calcification.
Figure 2: The resected specimen was a partial cystectomy specimen with perivesical fat and the median umbilical ligament.
Figure 3: A: Cyst with a smooth, whitish surface of 18X16X6 cm, to which is attached a gelatinous formation of 3X2 cm (in frame and in cartridge). B: Carcinomatous proliferation arranged in glandular structures and isolated cells, ring-like appearance, within pools of mucus. Infiltration of the detrusor muscle (star). Note a peri-nervous sheath (arrow) (Hematoxyllin Eosin x 250).
Microscopically, Carcinomatous proliferation arranged in glandular structures and isolated cells, ring-like appearance, within pools of mucus. Infiltration of the detrusor muscle (star) with peri-nervous sheath.
Malignant urachal neoplasms can arise from an urachal remnant but are rare and represent less than 1% of all bladder cancers yet 34% of all bladder adenocarcinomas are urachal in origin [1,2]. The urachus is lined by transitional epithelium, yet urachal carcinoma manifests as adenocarcinoma in 90% of cases. Urachal tumors are most commonly found in patients aged 40-70 years, and two-thirds of these cases occur in men [3]. The prognosis is related to the stage and degree of differentiation; however, due to their extraperitoneal location, they may be clinically silent and manifest only when invasion or metastatic disease occurs [3]. In these cases, prognosis is generally poor, with a 5-year survival rate of 6.5% - 15%.
- Thomas DG, Ward AM, Williams JL. A study of 52 cases of adenocarcinoma of the bladder. Br J Urol. 1971; 43: 4-15. PubMed: https://pubmed.ncbi.nlm.nih.gov/4926456/
- Sheldon CA, Clayman RV, Gonzalez R, Williams RD, Fraley EE. Malignant urachal lesions. J Urol 1984; 131: 1-8. PubMed: https://pubmed.ncbi.nlm.nih.gov/6361280/
- Mattelaer P, Wolff JM, Jung P, IJzerman W, Jakse G. Adenocarcinoma of the urachus: 3 case reports and a review of the literature. Acta Urol Belg 1997; 65: 63-67. PubMed: https://pubmed.ncbi.nlm.nih.gov/9175286/