More Information
Submitted: December 15, 2025 | Accepted: December 26, 2025 | Published: January 01, 2026
Citation: Ergun FU, Erdem MY, Cihan YB. The Role of Radiotherapy in Ovarian Serous Carcinoma with Leptomeningeal Metastasis: A Case Report Arch Case Rep. 2026; 10(1): 004-006. Available from:
https://dx.doi.org/10.29328/journal.acr.1001181
DOI: 10.29328/journal.acr.1001181
Copyright license: © 2026 Ergun FU, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ovarian cancer; Leptomeningeal metastasis; Radiotherapy
The Role of Radiotherapy in Ovarian Serous Carcinoma with Leptomeningeal Metastasis: A Case Report
Fatma Humeyra Ergun, Mehmet Yasin Erdem and Yasemin Benderli Cihan*
Department of Radiation Oncology, Kayseri City Education and Research Hospital, Kayseri, Turkey
*Corresponding author: Yasemin Benderli Cihan, Department of Radiation Oncology, Kayseri City Education and Research Hospital, Seker District, Muhsinyazıcıoglu Boulevard, No:77, 38080, Kocasinan, Kayseri, Turkey, Email: [email protected]
Ovarian cancer accounts for 4% of all cancers in women and very rarely metastasizes to the leptomeningeal region. Recent advances in systemic treatment options and the resulting increase in survival have led to an increase in central nervous system metastases. Radiotherapy plays a crucial role in the multidisciplinary management of leptomeningeal metastases. This study will discuss a case of serous ovarian carcinoma that presented to our clinic with leptomeningeal metastases two years after surgery and adjuvant chemotherapy, for which we administered palliative radiotherapy.
Ovarian cancer accounts for 4% of cancers in women and 25% of gynecological cancers in women. It is the leading cause of cancer-related death in women worldwide. More than 90% are epithelial neoplasms, and serous carcinoma is the most common subtype [1,2]. Most cases are diagnosed at an advanced stage of development. Ovarian cancer metastasizes primarily to the peritoneum, but most commonly to the small intestines, liver, and lungs. Metastasis to the brain and meninges occurs in approximately 0.06% of cases [3].
Leptomeningeal metastasis (LM) is the spread of cancer cells from the primary tumor to the pia mater, arachnoid mater, cerebrospinal fluid, and spinal cord [4]. Leptomeningeal metastases occur late in 5% - 8% of solid tumors. While melanoma, lung, and breast cancers most commonly metastasize to the leptomeninges, this condition is very rare in gynecological cancers. LM is associated with a poor prognosis [4].
Radiation therapy (RT), in addition to intrathecal chemotherapy and systemic chemotherapy, plays an important role in the multidisciplinary treatment of patients with LM. It is administered for palliative purposes, to prevent neurological symptoms, and to stabilize the disease [5].
A case presented to our clinic with leptomeningeal metastases 2 years after diagnosis, for which we performed palliative radiotherapy, will be discussed, along with a literature review.
A 70-year-old woman with a history of five pregnancies and a live birth presented to the obstetrics and gynecology outpatient clinic in 2022 with complaints of abdominal distension. Probe curettage results were suspicious, and she underwent TAH-BSO and omentectomy. According to the American Joint Committee on Cancer (AJCC) (8th ed., 2017) staging system, the patient was assessed as stage IIIC ovarian serous carcinoma. After surgery, the patient received six cycles of carboplatin and paclitaxel treatment by medical oncology, and she was followed up.
In 2024, 3 months after her last chemotherapy treatment, she developed a headache, nausea, and vomiting. The patient presented to our hospital’s emergency department after experiencing difficulty walking and speaking, bilateral weakness in the lower extremities, and increasing headaches. A contrast-enhanced cranial magnetic resonance imaging (MRI) revealed multiple metastatic foci scattered throughout the brain. After evaluation by a neurosurgeon, the patient was referred to our clinic.
On admission to physical examination, the patient had a Glasgow coma score of 15, was in fair general condition, was conscious, oriented, cooperative, and immobile, and had normal sensory and cranial nerve examinations. There was no neck stiffness. Motor examination revealed muscle strength of 5/5 bilaterally in the upper extremities and 3/5 bilaterally in the lower extremities. A brain MRI suggested a preliminary diagnosis of leptomeningeal metastasis, meningitis, or parasitic infection. Contrast-enhanced cervical, thoracic, and lumbar spinal MRIs were requested. The patient was then consulted with neurosurgery and infectious diseases. Based on the infectious disease laboratory results and physical examination, the neurosurgeon ruled out an infectious disease. Surgery was not recommended. Contrast-enhanced spinal MRI confirmed leptomeningeal metastases. The lesions were primarily evaluated by radiology as ovarian cancer metastases. The patient was given palliative whole-brain radiotherapy (WBRT) and focal spinal radiotherapy (FSRT). Because of the presence of edema around the masses throughout the central nervous system, IV dexamethasone was initiated. WBRT with a photon energy of 6 MV was administered via the LINAC device, with 14 Gy (2 x 7 Gy) delivered to the affected areas around the spinal cord (C2-C3, T4-T8, and T12-L1 levels), followed by 20 Gy in four fractions.
Follow-up showed improvement in the patient’s general condition. Her headaches subsided. She was referred to medical oncology for chemotherapy. One course of Paclitaxel + Carboplatin + Bevacizumab was administered on November 20, 2024. On control contrast-enhanced cranial MRI, multiple lesions were observed in the cerebellar hemispheres, the most prominent of which was 11 mm in diameter, and in the cerebral hemispheres, the most prominent was 17 mm in the right temporal lobe and 13 mm in the left parietal region. These lesions were rare in the cerebral hemispheres and more frequent in the deep white matter of the cerebral hemispheres, with edema appearing in patches on the periphery. In the following days, the patient developed a systemic infection and was admitted to the intensive care unit. The patient died on December 10, 2024.
Leptomeningeal metastases are a rare condition, occurring in 5-8% of solid tumors [4]. Breast, lung cancers, and malignant melanoma are the most common solid tumors causing LM. The mechanism of leptomeningeal metastases involves hematogenous spread of tumor cells from the primary tumor site, direct seeding from a metastatic site in the brain or spinal cord parenchyma that is in contact with the CSF, direct spread from subdural or extradural tumors, or direct spread from regions outside the central nervous system and adjacent to it [3].
In the presented case, no metastases were observed in the lungs, bones, or abdomen on restaging imaging. It was suspected that LM had spread hematogenously from the pelvic venous vessels, commonly seen in pelvic tumors, to the vertebral venous plexus (Batson’s Plexus), and from there to the leptomeninges.
The most common symptoms of LM are headache, followed by nausea and vomiting, limb weakness, ataxia, and confusion [4]. In our case, the primary findings were headache, nausea and vomiting, and loss of motor strength in the lower extremities.
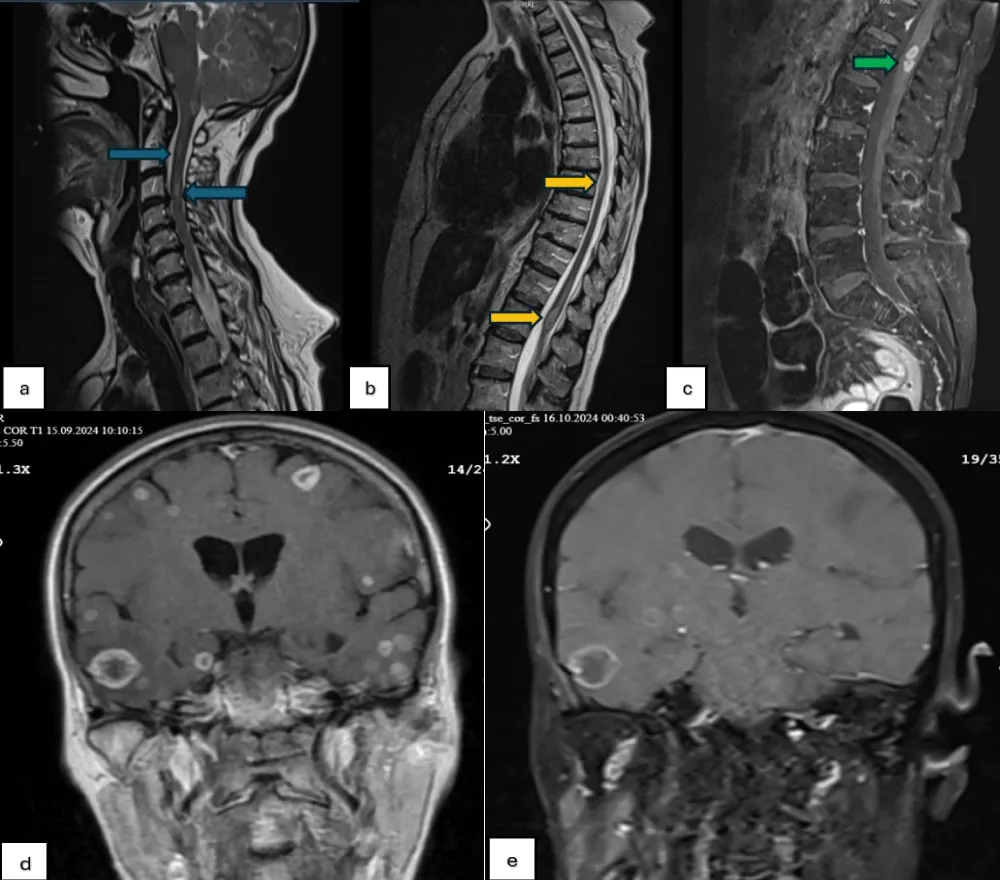
The diagnosis of LM is primarily made after a comprehensive history and physical examination, followed by brain and cervical-thoracic-lumbar spinal MRI, and cerebrospinal fluid (CSF) analysis. Diffuse and focal contrast enhancement on T1-weighted contrast-enhanced MRI is the typical appearance and is the primary diagnostic tool for LM [3,6]. As in the case presented here, a non-enhancing mass may also appear on T1-weighted images. Contrast-enhanced FLAIR sequences are more sensitive in detecting LM in these cases [3]. Contrast enhancement on MRI is seen in both LM and inflammatory meningitis. CSF sampling should be used to differentiate [7]. A lumbar puncture was not performed in our case due to the short expected survival time and the risk of herniation of the space-occupying lesion in the brain as a result of the lumbar puncture (Figure 1).
Figure 1: (a-c) Dural metastases with nodular enhancement along the spinal cord on T1- and T2-weighted MRIs, (d): Extensive metastases in the brain on pre-RT T1-weighted MRI, (e) Extensive metastases in the brain on post-RT T1-weighted MRI.
Differential diagnosis should include meningitis or encephalitis caused by various organisms, primary brain lesions, autoimmune and vascular diseases, and paraneoplastic syndromes [4]. In our case, the eosinophil count was 100 cells/mcL, thus ruling out a diagnosis of parasitic infection. The patient’s lack of a history of tuberculosis and normal vital signs also ruled out bacterial infections. Whole-brain RT should be the primary treatment option for patients who do not require urgent decompression and whose brain metastases are too extensive for surgical intervention. Various dose fractionations are accepted for WBRT. The two most commonly used treatment schedules are 30 Gy in 10 fractions or 20 Gy in 5 fractions. Shorter schedules of 10 Gy in a single fraction or 12 Gy in 2 fractions can also be applied [5]. In our patient, we approached whole-brain irradiation for a total of 14 Gy in 2 fractions. Radiotherapy for lesions around the spinal cord can be administered comprehensively as craniospinal or as involved field radiotherapy (IFRT) applied only to symptomatic areas [5]. However, it should be noted that leptomeningeal disease is a diffuse condition, and focal RT is a temporary solution [5]. Limited data are available on IFRT dose fractionation. According to previous studies, doses range from 20 to 40 Gy in 5-20 fractions. In our patient, 4 x 5 Gy RT was administered to the affected areas around the spinal cord.
In recent years, new treatment modalities have prolonged the survival of cancer patients. Consequently, patients are rarely presented with metastatic conditions. Leptomeningeal metastases should be considered when advanced cancer patients present with various neurological symptoms. Furthermore, it is important to remember that RT plays an important role in the palliative approach to LM treatment management.
- Rosen DG, Yang G, Liu G, Mercado-Uribe I, Chang B, Xiao XS, et al. Ovarian cancer: pathology, biology, and disease models. Front Biosci. 2009;14:2089-2102. Available from: https://www.imrpress.com/journal/FBL/14/5/10.2741/3364
- Tahir N, Ram A, Jain N, Vemireddy LP, Zahra F. Leptomeningeal carcinomatosis in epithelial ovarian cancer: a diagnostic challenge. Cureus. 2021;13(4):e14440. Available from: https://www.cureus.com/articles/55953
- Uchikura E, Fukuda T, Imai K, Yamauchi M, Kasai M, Ichimura T, et al. Carcinomatous meningitis from ovarian serous carcinoma: a case report. Oncol Lett. 2022;25(2):66. Available from: https://www.spandidos-publications.com/10.3892/ol.2022.13652
- Batool A, Kasi A. Leptomeningeal carcinomatosis. [Updated 2023 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499862/
- Barbour AB, Zaki P, McGranahan TM, Venur V, Vellayappan B, Palmer J, et al. Emergent radiotherapy for brain and leptomeningeal metastases: a narrative review. Ann Palliat Med. 2023;12(6):1405-1419. Available from: https://apm.amegroups.org/article/view/108771
- Nguyen A, Nguyen A, Dada OT, Desai PD, Ricci JC, Godbole NB, et al. Leptomeningeal metastasis: a review of the pathophysiology, diagnostic methodology, and therapeutic landscape. Curr Oncol. 2023;30(6):5906-5931. Available from: https://www.mdpi.com/1718-7729/30/6/442
- Anwar A, Gudlavalleti A, Ramadas P. Carcinomatous meningitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560752/