More Information
Submitted: December 15, 2025 | Accepted: December 24, 2025 | Published: December 26, 2025
Citation: Erdem MY, Turker Y, Cihan YB. Primary Cutaneous B-cell Lymphoma with Widespread Involvement: Case Report. Arch Case Rep. 2025; 9(12): 409-411. Available from:
https://dx.doi.org/10.29328/journal.acr.1001179
DOI: 10.29328/journal.acr.1001179
Copyright license: © 2025 Erdem MY, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Non-Hodgkin lymphoma; Primary cutaneous lymphoma; Radiotherapy; B-cell lymphoma
Primary Cutaneous B-cell Lymphoma with Widespread Involvement: Case Report
Mehmet Yasin Erdem, Yusuf Turker and Yasemin Benderli Cihan*
Kayseri City Education and Research Hospital, Department of Radiation Oncology, Kayseri, Turkey
*Corresponding author: Yasemin Benderli Cihan, MD, Kayseri City Education and Research Hospital, Department of Radiation Oncology, Kayseri, Turkey, Email: [email protected]
Primary cutaneous lymphomas (PCL) are extranodal non-Hodgkin lymphomas affecting the skin without other systemic involvement at the time of diagnosis. Our case was a 62-year-old patient with PCBLC who had deep and multiple skin involvement but no systemic symptoms or involvement. At diagnosis, there was widespread skin involvement of the anterior chest wall, more pronounced on the left side. The patient received RT at 30 Gy/17 fractions for the lesions located on the anterior chest wall and 20 Gy/11 fractions as a boost to the primary mass. Six months after treatment, the patient demonstrated a near-complete response. In this case report, a case of primary B-cell cutaneous lymphoma with widespread chest wall involvement, which achieved a complete response to RT, is discussed with the literature.
Primary cutaneous lymphomas (PCL) are extranodal non-Hodgkin lymphomas that affect only the skin and do not show systemic involvement at the time of diagnosis. Primary cutaneous B-cell lymphomas (PCBCL) constitute approximately 25% of all PCLs and are a relatively rare group [1]. They are more common in patients over 60 years of age and in males. While the etiology is not fully understood, advanced age and viral infections such as EBV, HHV-8, HIV, and HCV are thought to be predisposing factors. Clinically, they present as patches, plaques, and non-ulcerated nodules; they may exhibit solitary or multifocal involvement [2]. Diagnosis is made by incisional, excisional, or punch biopsy involving the reticular dermis and subcutaneous fat [3].
Therapeutic approach: It should be determined based on clinical, histopathological, phenotypic, genetic, and prognostic factors, requiring a multidisciplinary approach involving a dermatologist, hematologist, pathologist, medical oncologist, and radiation oncologist [4]. Surgery, radiotherapy, and chemotherapy are among the treatment options, but PCBCLs are generally indolent, with a 5-year survival rate of approximately 90% [2]. In this case report, a case of PCBCL with extensive chest wall involvement that achieved a complete response to radiotherapy is discussed, along with the literature.
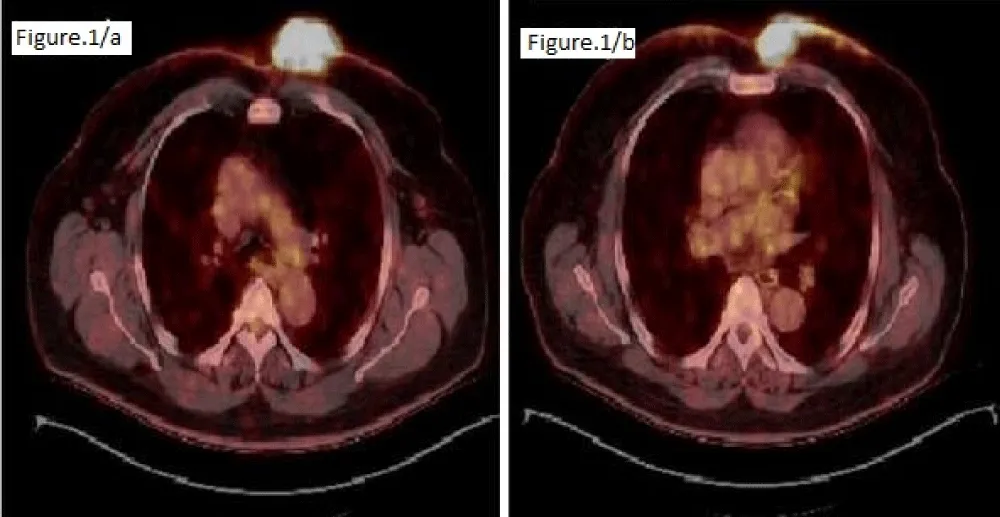
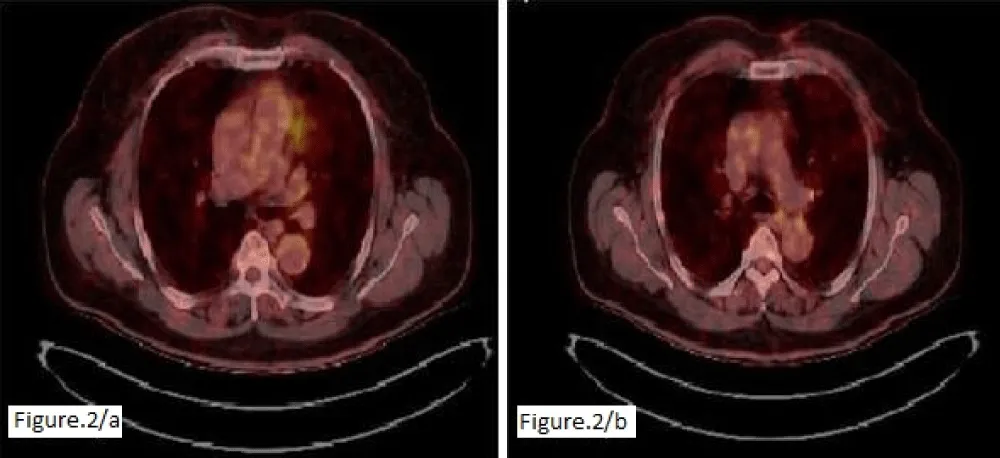
A 65-year-old man presented to the dermatology clinic with complaints of a large erythematous plaque on the anterior chest that had been gradually increasing for two months. He had a history of gout, hypertension, and inflammatory bowel disease, and a history of renal cystectomy and lumbar disc herniation. A biopsy revealed atypical lymphoid infiltration consistent with CD5-negative non-Hodgkin’s B-cell lymphoma, with diffuse CD20 positivity, focal BCL-6 and CD10 positivity, and negative CD34, CD117, TDT, and p63 positivity, extending from the superficial dermis to the subcutaneous fat. The patient was referred to the hematology department. The patient, who had no symptoms, had a PET-CT scan of the left hemithorax. A 57 x 74 mm irregular mass infiltrating the skin/subcutaneous tissue and bilateral (prominent on the left) multifocal skin thickening reaching approximately 9 mm on the anterior chest wall was observed (Figure 1). No systemic involvement was detected, and the patient was referred for RT without considering chemotherapy, phototherapy, or cryotherapy. The patient was treated with the Linac device using an intensity-modulated RT technique using 6 MV photon energy. A boost of 30 Gy/17 fractions was applied to the extensive lesions on the anterior chest wall, and a boost of 20 Gy/11 fractions was applied to the primary mass. Post-treatment physical examination revealed marked regression of the mass and disappearance of the erythematous lesions. A one-month CT scan revealed marked regression of the primary mass and a complete response in the smaller lesions. Six months later, the lesions were reported to have completely disappeared (Figure 2).
Figure 1: Intense hypermetabolic activity corresponding to irregular areas of thickening with focal nodular formations in the cutaneous tissue of the anterior chest wall, more prominent on the left side.
Figure 2: PET-CT image obtained at the 6th month after RT; no hypermetabolic nodular formations were observed.
PCL is a rare disease group with diverse phenotypic, clinical, and genetic characteristics. The recent increase in its incidence is related to the widespread availability of diagnostic tools and the early detection of skin involvement [1]. In a study of 8,593 cases by Dobos, et al. PCL was most commonly seen in men over 60 years of age, with an incidence of 1.06/100,000 [6]. Our case was a 63-year-old male, consistent with the literature. Following diagnosis, a complete blood count, biochemical tests including LDH, and electrophoresis and flow cytometry should be performed in appropriate patients. Although it is an indolent B-cell lymphoma, radiologic/nuclear imaging is necessary to assess for possible systemic involvement. A bone marrow biopsy should be performed in high-risk cases.
The treatment choice for PCLCL depends on the location, number, size, and subtype of the lesion. Phototherapy or cryotherapy is preferred for superficial lesions, while RT is the preferred treatment for deep-seated lesions [5,7]. In our case, RT was chosen due to the deep and large size of the lesion.RT is one of the most effective treatment methods, especially for localized lesions, but recurrence rates can range from 25% - 63% [5]. Because lymphocytes are radiosensitive, RT is an especially effective option for deep plaques and tumors [7]. The EORTC recommends 40 Gy/20 fractions of RT for primary cutaneous large B-cell lymphomas [8]. Different RT dose regimens have been reported in the literature. Elsayad et al. recommended 40 Gy (2 Gy/fx) or 16 Gy (4 Gy/fx) for PKBCL and 4 Gy (2 Gy/fx) or 20 Gy (2 Gy/fx) regimens for more indolent subtypes with multifocal involvement [8]. Ceovic et al. reported no recurrence after 15 Gy in multifocal primary cutaneous marginal zone lymphoma during a 12-month follow-up [9]. Our case was a rapidly progressing PCLCL with a large nodular lesion accompanied by smaller lesions on the opposite side. Therefore, 30 Gy of RT was administered to the anterior chest wall, followed by an imaging-guided boost to the primary mass, totaling 50 Gy. A complete response was achieved after treatment.
PCLCL generally has a good prognosis, but early recurrence can occur depending on the subtype [10]. Factors such as age, performance status, B symptoms, phenotype, and systemic involvement influence prognosis. Liao, et al. reported early recurrence and mortality in a patient with advanced age and excision who could not undergo RT [11]. Although the subtype in our case could not be clearly determined by biopsy, the early complete response to RT suggests a favorable prognosis.
Primary cutaneous B-cell lymphomas are a rare group of indolent lymphomas affecting the skin without systemic involvement. A multidisciplinary approach is essential for diagnosis and treatment. In the presence of deep and nodular lesions, radiotherapy is an effective and well-tolerated treatment option. In the presented case, despite widespread chest wall involvement, the complete response achieved with RT supports the effectiveness of RT in the treatment of PCLCL with appropriate dose and technique.
- Vermeer M. Epidemiology of cutaneous lymphoma. Br J Dermatol. 2021;184(6):993. Available from: https://doi.org/10.1111/bjd.19829
- Lima M. Cutaneous primary B-cell lymphomas: from diagnosis to treatment. An Bras Dermatol. 2015;90(5):687. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4631235/
- Hristov AC, Tejasvi T, Wilcox RA. Cutaneous B-cell lymphomas: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol. 2023;98(8):1326–1332. Available from: https://doi.org/10.1002/ajh.26968
- Chilom DS, Farcaș SS, Andreescu NI. Primary cutaneous B-cell lymphoma co-existing with mycosis fungoides: a case report and overview of the literature. Life (Basel). 2022;12(12):2067. Available from: https://doi.org/10.3390/life12122067
- Di Stefani A, Tagliaferri L, Lancellotta V, Fionda B, Fossati B, Balducci M, et al. The safety of radiotherapy in the treatment of primary cutaneous B-cell lymphoma: a multidisciplinary systematic review. Front Oncol. 2020;10:1133. Available from: https://doi.org/10.3389/fonc.2020.01133
- Dobos G, de Masson A, Ram-Wolff C, Beylot-Barry M, Pham-Ledard A, Ortonne N, et al. Epidemiological changes in cutaneous lymphomas: an analysis of 8593 patients from the French Cutaneous Lymphoma Registry. Br J Dermatol. 2021;184(6):1059–1067. Available from: https://doi.org/10.1111/bjd.19644
- Kouhen F, Oqbani K, Gouach H El, Ahnach M, Dahbi Z. Overcoming chemotherapy resistance in cutaneous T-cell lymphoma: a successful case of high-dose radiotherapy management. Cureus. 2023;15(8):e43959. Available from: https://doi.org/10.7759/cureus.43959
- Elsayad K, Guenova E, Assaf C, Nicolay JP, Trautinger F, Stadler R, et al. Radiotherapy in cutaneous lymphomas: recommendations from the EORTC cutaneous lymphoma tumour group. Eur J Cancer. 2024;212:115064. Available from: https://doi.org/10.1016/j.ejca.2024.115064
- Ceovic R, Jovanovic I, Kostovic K, Rados J, Dotlic S, Radman I, et al. Radiotherapy of primary cutaneous follicle center lymphoma: case report and review of literature. Radiat Oncol. 2013;8(1):147. Available from: https://doi.org/10.1186/1748-717x-8-147
- Pinter-Brown LC. Diagnosis and management of cutaneous B-cell lymphoma. Dermatol Clin. 2015;33(4):835–840. Available from: https://doi.org/10.1016/j.det.2015.05.003
- Liao C, Yang M, Liu P, Zhang W. A 92-year-old man with primary cutaneous diffuse large B-cell non-Hodgkin’s lymphoma manifesting as a giant scalp mass: a case report. Medicine (Baltimore). 2017;96(10):e6270. Available from: https://doi.org/10.1097/md.0000000000006270