More Information
Submitted: November 05, 2025 | Approved: November 10, 2025 | Published: November 11, 2025
How to cite this article: Parzefall J, Girotti P, Weigl MP, Hanewald L, Königsrainer I. Whipple Procedure in a Patient with Duplicated Portal Vein and other Major Abnormalities in Vascular Anatomy of the Upper Abdomen – A Case Report of a Rare Finding. Arch Case Rep. 2025; 9(11): 366-369. Available from:
https://dx.doi.org/10.29328/journal.acr.1001174
DOI: 10.29328/journal.acr.1001174
Copyright license: © 2025 Parzefall J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Whipple Procedure in a Patient with Duplicated Portal Vein and other Major Abnormalities in Vascular Anatomy of the Upper Abdomen – A Case Report of a Rare Finding
Jürgen Parzefall *, Paolo Girotti, Markus Philipp Weigl, Lars Hanewald and Ingmar Königsrainer
*, Paolo Girotti, Markus Philipp Weigl, Lars Hanewald and Ingmar Königsrainer
Lindenweg 17, 6830 Rankweil, Austria
*Address for Correspondence: Jürgen Parzefall, Lindenweg 17, 6830 Rankweil, Austria, Email: [email protected]
We present the case of a patient with a duplicated portal vein, a duplicated inferior vena cava, and an arterial hepatic blood supply with a single aberrant left hepatic artery. Due to carcinoma of the pancreatic head, a Whipple Procedure was performed. There were no intra- or postoperative complications, and the patient is currently in good condition with no evidence of recurrence of disease in the one-year follow-up.
Whipple procedure with locoregional lymphadenectomy is the gold standard treatment for adenocarcinoma of the pancreatic head. The correlation between the tumour and the portal vein, as well as the other major visceral vessels, is a main criterion defining operability [1]. Variation of vascular anatomy may influence operability or surgical strategy.
In the embryological period, the portal vein develops from the vitelline vein system, and the vena cava superior et inferior develop from the cardinal vein system. Both systems primarily originate as a pair of right and left veins, which are connected to each other with anastomotic veins. During the developmental process, those veins partly disappear and partly fuse, leading to the mature form of vascular anatomy we all know [2]. Despite the complexity of this process, variation in the extrahepatic course of the portal vein as well as the venae cavae is rare [3]. In contrast, the arterial blood supply of the liver shows high variation [4].
In the following, we will describe a case of a patient with a duplication of the portal vein as well as other rare vascular abnormalities in the upper abdomen, in which we performed a Whipple procedure due to adenocarcinoma of the pancreatic head.
In October 2024, a 77-year-old male patient with adenocarcinoma of the pancreatic head was discussed on the oncological board in the regional hospital in Feldkirch, Austria.
To define operability, the relation between the tumour and the main vessels was investigated in the CT scan. A whole list of anatomical abnormalities was observed:
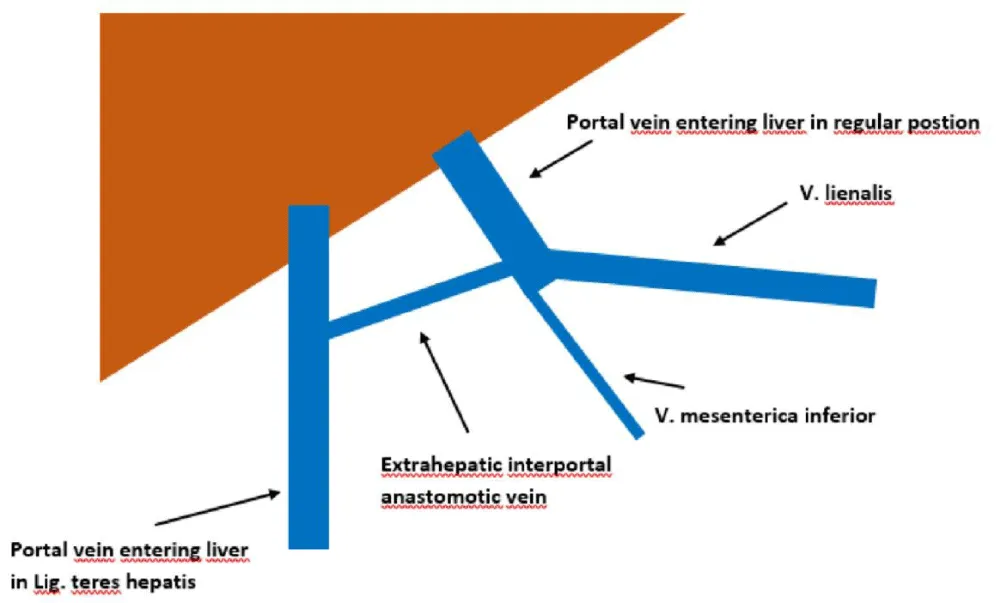
Duplicated portal vein:
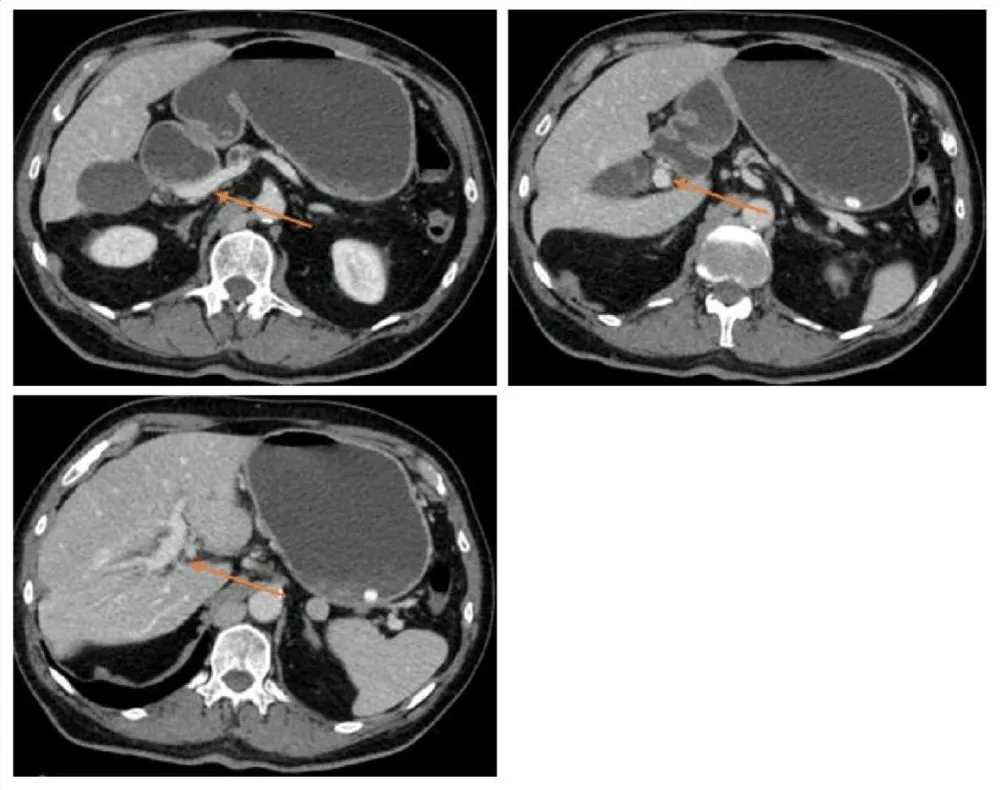
- portal vein in regular position, formed from the inferior mesenteric vein and the splenic vein, supplying segment III, IVb, and V (Figures 1,2).
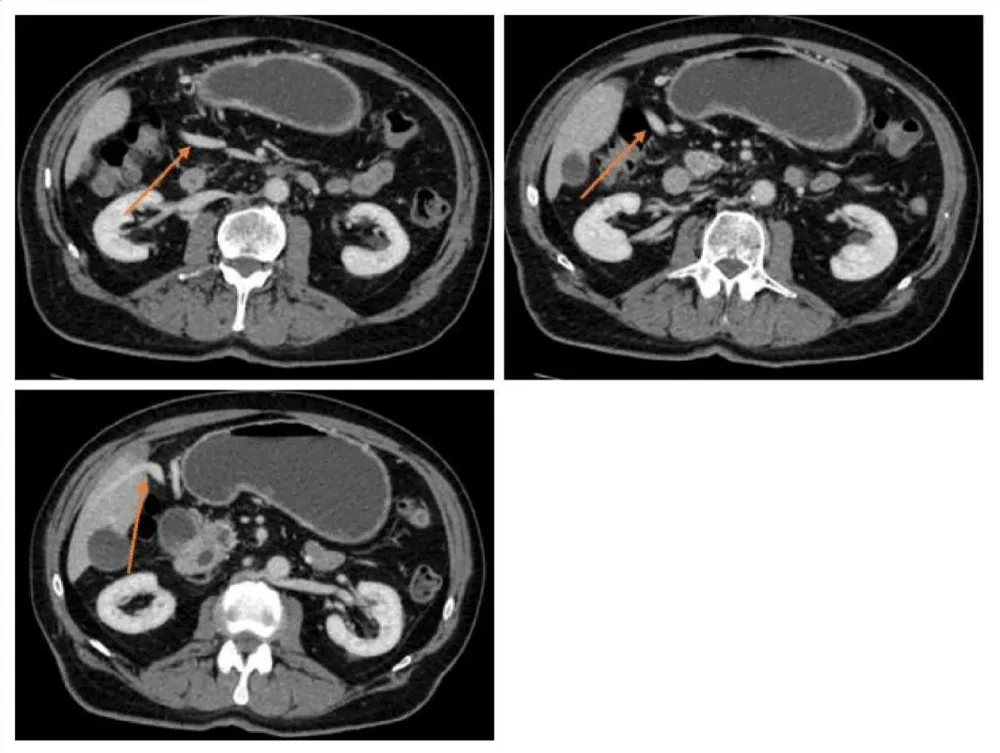
- portal vein, which forms from the superior mesenteric vein entering the liver in the ligamentum teres hepatis, supplying the other segments (Figure 3).
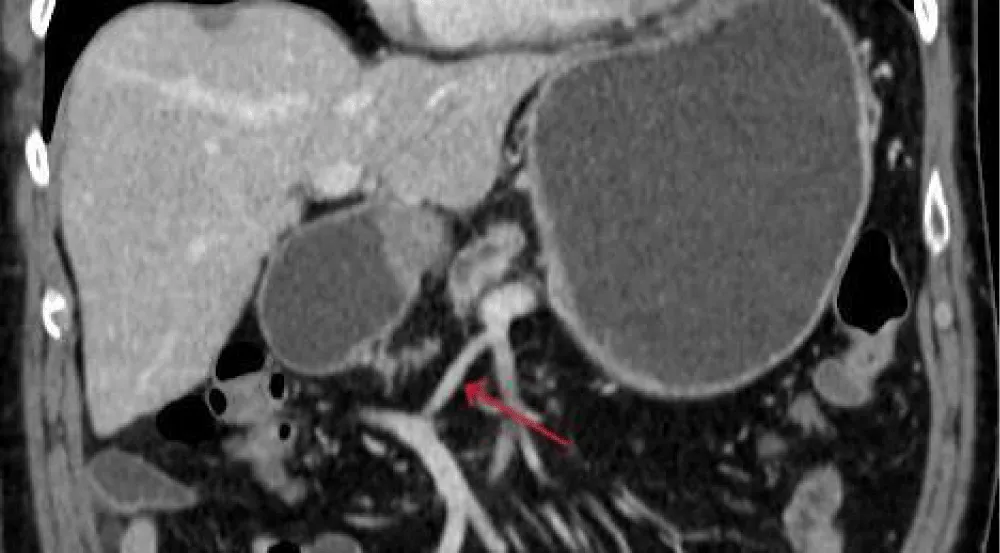
- Both portal veins are connected extrahepatically via a 3 cm anastomotic vein (Figure 4).
Figure 1: Schematic depiction of the anatomical variation of the extrahepatic portal vein in the presented case.
Figure 2: CT scan presenting the first portal vein forming from V. mesenterica inferior and V. lienalis.
Figure 3: CT scan presenting a second portal vein forming from V. mesenterica superior, entering the Liver via the ligament. Teres hepatis.
Figure 4: CT scan presenting the extrahepatic interportal anastomotic vein.
Two inferior vena cavae are present:
- Forming from each iliac vein, dorsally passing the liver as well as the heart, draining into the superior vena cava via the V. azygos
- A short inferior vena cava, formed from the confluence of the hepatic veins, drains directly into the right atrium
- No common hepatic artery in the hepatoduodenal ligament
- The arterial blood supply of the liver via a single left aberrant hepatic artery
No contraindication for surgery was present. Necessary modifications in the surgical approach due to the different anatomy were discussed and declared possible. Hence, the tumour was declared operable in the oncological board, and the patient was evaluated for primary surgery. After properly preparing the patient, the Whipple procedure was performed on the 26th of November 2024.
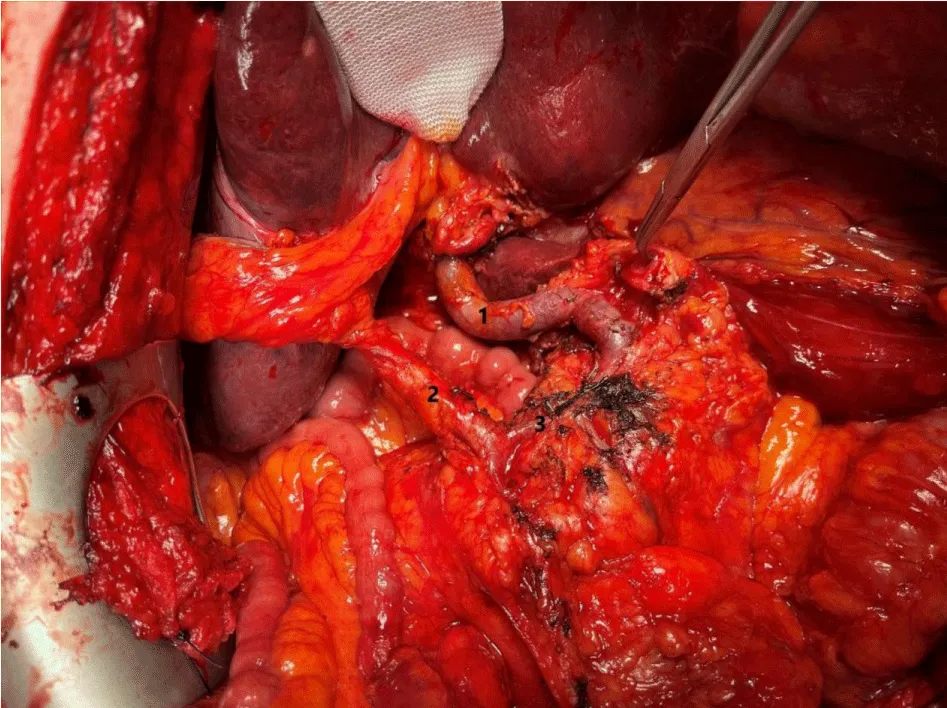
Intraoperative findings confirmed the major vascular abnormalities: After Kocher’s manoeuvre, the lesser sac was opened. In contrast to the regular surgical approach, as a next step, the accessory portal vein had to be dissected. Starting from ligamentum teres hepatis, proceeding along the upper margin of the pancreas, and finishing in the mesenteric root. Using the knowledge of anatomy from the CT scan, no surgical complication occurred during this extra step. Now the superior mesenteric artery was dissected and showed no infiltration of the tumor. The ligamentum hepatoduodenale with the small portal vein and the ductus hepatocholedochus were dissected, as well as the accessory left hepatic artery. After cholecystectomy, the right gastric and the gastroduodenal artery were transected. The jejunum was cut 40 centimetres after Treitz. The pancreas was transected, preserving the regular portal vein, the accessory portal vein, and the superior mesenteric artery. After transection of the stomach, reconstruction was performed regularly, and the Whipple procedure was completed. Situs after resection is shown in Figure 5.
Figure 5: Situs after resection; 1 regular portal vein; 2 accessory portal vein; 3 extrahepatic anastomotic vein.
Histological examination showed an adenocarcinoma of the pancreatic head. TNM Classification was grade 2 pT2 N1 R0. The postoperative course was without any complications. The patient could be sent home on the 9th day after surgery in good condition. Adjuvant chemotherapy was performed, and the patient is still in good condition. A one-year follow-up investigation did not show any sign of recurrence of disease.
Normally, the portal vein forms from the confluence of the superior mesenteric vein and the splenic vein dorsal to the pancreatic neck and continues along the hepatoduodenal ligament into the liver. In approximately 20% of cases, the inferior mesenteric vein also drains directly into the confluence [5]. Other variations of the extrahepatic portal vein are rare and described, such as the preduodenal portal vein, postduodenal-prepancreatic portal vein (PPPV), prebiliary portal vein, and cavernous transformation of the portal vein [3]. Duplication of the portal vein is only described in a few case reports [6-9].
Literature research did not show any other case where the Whipple procedure was performed in a patient with a duplicated portal vein. Hence, comparison with other cases is difficult.
One case report could be found where a Whipple procedure was performed in a patient with duplicated vena cava as well as intrahepatic trifurcation of the portal vein. No perioperative complications occurred in this case. However, in contrast to our case, the extrahepatic anatomy of the portal vein was normal [10].
Another case report described the Whipple procedure in a patient with a PPPV. In this case, massive intraoperative bleeding from the PPPV led to its resection and reconstruction using an autogenous graft [11].
In another case, a patient underwent an elective laparoscopic cholecystectomy. Due to rupture of the portal vein, conversion to open reconstruction of the portal vein had to be performed. Cavernous transformation of the portal vein could be identified and was very likely the reason for the complication [12].
Portal vein duplication is an extremely rare anatomical variant. Its combination with an indication for the Whipple procedure is so rare that no other case has been reported so far.
Other cases showed that variation of portal vein anatomy can be a challenge for hepatopancreatic surgeons, especially if the anatomical situation is not clear preoperatively.
With this case, it could be shown that if preoperative investigation of vascular anatomy is done assiduously, major vascular abnormalities as described in this case are not only not contraindication for oncological surgery but can be performed with comparable intraoperative risk as in patients with regular vascular anatomy.
- Grossberg AJ, Chu LC, Deig CR, Fishman EK, Hwang WL, Maitra A, et al. Multidisciplinary standards of care and recent progress in pancreatic ductal adenocarcinoma. CA Cancer J Clin. 2020 Sep;70(5):375-403. Available from: https://doi.org/10.3322/caac.21626
- Collardeau-Frachon S, Scoazec J. Vascular development and differentiation during human liver organogenesis. Anat Rec. 2008 Jun 16;291(6):614-27. Available from: https://doi.org/10.1002/ar.20679
- Marks C. Developmental basis of the portal venous system. Am J Surg. 1969 May;117(5):671-81. Available from: https://doi.org/10.1016/0002-9610(69)90404-8
- Zaki SM, Abdelmaksoud AHK, Khaled BEA, Abdel Kader IA. Anatomical variations of the hepatic artery using the multidetector computed tomography angiography. Folia Morphol (Warsz). 2020;79(2):247-54. Available from: https://doi.org/10.5603/fm.a2019.0090
- Layton BM, Lapsia SK. The portal vein: A comprehensive review. Radiographics. 2023 Nov;43(11):e230058. Available from: https://doi.org/10.1148/rg.230058
- Yang Q, Li J, Wang H, Wang S. A rare variation of duplicated portal vein: left branch derived from splenic vein mimicking cavernous transformation. BMC Gastroenterol. 2021 Oct 26;21(1):404. Available from: https://doi.org/10.1186/s12876-021-01970-8
- Du G, Li J, Qi Y. An unusual developmental anomaly of duplicated portal vein. Folia Morphol (Warsz). 2024;83(3):737-9. Available from: https://doi.org/10.5603/fm.97785
- Kitagawa S. Anomalous duplication of the portal vein with prepancreatic postduodenal portal vein. J Rural Med. 2022 Oct;17(4):259-61. Available from: https://doi.org/10.2185/jrm.2022-009
- Liu G, Song L, Li Y, Jiang L. Three main portal veins: A very rare case of portal vein anomaly. J Clin Imaging Sci. 2024;14:41. Available from: https://doi.org/10.25259/jcis_107_2024
- Chrysikos D, Delis S, Smerdi D, Charitaki E, Solia E, Troupis T. Duplicated inferior vena cava-trifurcated portal vein: a rare anatomical variation encountered during Whipple procedure. J Surg Case Rep. 2023 Jan;2023(1):rjad014. Available from: https://doi.org/10.1093/jscr/rjad014
- Higashihara T, Morita Y, Hayashi T, Takahashi M, Yogi N, Sasaki S, et al. Hepatobiliarypancreatic surgery for patients with a prepancreatic postduodenal portal vein: a case report and literature review. BMC Surg. 2022 Dec 13;22(1):55. Available from: https://doi.org/10.1186/s12893-022-01508-z
- Frankowska A, Kobryń K, Rykowski P, Gibiński K, Grąt M. Challenges of duplicated portal vein in elective laparoscopic cholecystectomy: a case report. Am J Case Rep. 2025 Mar 14;26.e946151. Available from: https://doi.org/10.12659/ajcr.946151