More Information
Submitted: June 10, 2025 | Approved: June 16, 2025 | Published: June 17, 2025
How to cite this article: Sena-Martins M, Tadini V, Nakata TY, Borges JD, Netto MJBR, Reis N, et al. Case Report: Fundal Hysterotomy in Pregnant Woman after Augmentation Cystoplasty. Arch Case Rep. 2025; 9(6): 201-203. Available from:
https://dx.doi.org/10.29328/journal.acr.1001146
DOI: 10.29328/journal.acr.1001146
Copyright license: © 2025 Sena-Martins M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Augmentation cystoplasty; Case report
Case Report: Fundal Hysterotomy in Pregnant Woman after Augmentation Cystoplasty
Sena-Martins M*, Tadini V, Nakata TY, Borges JD, Netto MJBR, Reis N, Piantavinha BB, Costa LR, Sampaio MCB, Rabelo MEP and Souza GN
Campinas, SP, Brazil
*Address for Correspondence: Sena-Martins M, Campinas, SP, Brazil, Email: [email protected]
Cesarean section in a fundal hysterotomy was a rare obstetric procedure in the past but its use has increased largely due to changes in the approach to complex cesarean deliveries, particularly in cases where the lower uterine segment incision is not feasible and adjacent organs surgeries (bowel, bladder) somehow interfere with the execution of the standard operation. There are many indications that justify the boost in its practice, including difficult access to the lower uterine segment (due to the presence of fibroids or placenta accreta spectrum), challenging fetal extraction during the cesarean section, or injury to adjacent organs as a result of adhesions or bladder augmentation through cystoplasty procedures. This paper may contribute to and advise surgeons to decrease injuries in pregnant patients with previous bladder augmentation surgery. Ruan J, Zhang L, Duan MF, Luo DY [1]; Vordermark JS [2]; Shaikh A, Ahsan S, Zaidi Z [3]; Hensle TW, Bingham JB, Reiley EA, et al. [4]; Taniguchi A, Kakizaki H, Murakumo M, Nonomura K, Koyanagi T [5].
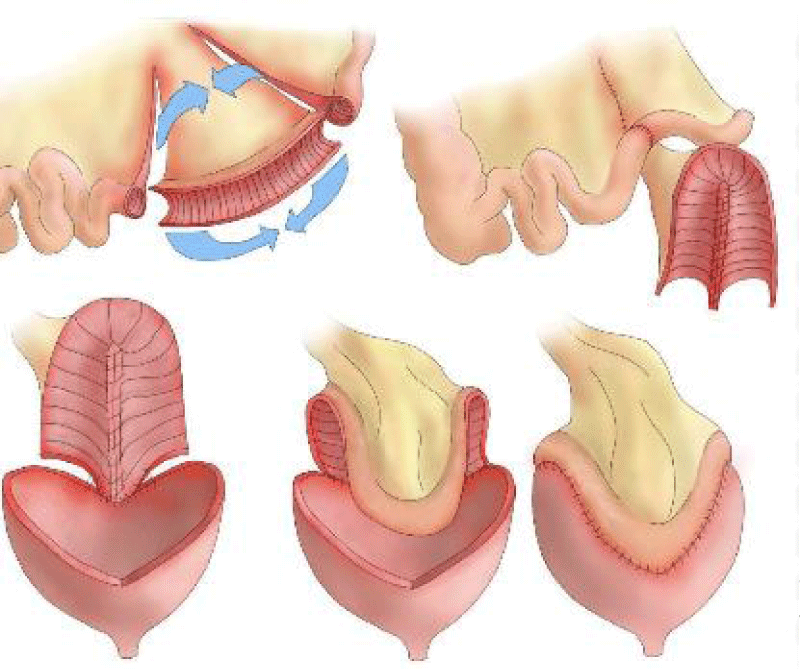
Bladder augmentation surgery is a surgical treatment option for myelomeningocele aimed at reducing episodes of incontinence, urinary tract infections, and kidney complications. It involves the use of intestinal or stomach segments to increase bladder capacity in individuals with inadequate function, such as low bladder compliance. The most commonly used intestinal segment is an ileal or ileocecal patch, while the sigmoid colon is the least commonly used. This procedure was first described by Mikulicz in 1899 and became widely adopted in the 1970s after the dissemination of clean intermittent self-catheterization. Vordermark JS, Deshon GE, Agee RE [6]; Hill, D. E., & Kramer, S. A. [7]; Greenwell TJ, Venn SN, Creighton S, et al. [8]; Kapoor D, Chipde SS, Agrawal S, et al. [9]. Breen M; Phelps A; Estrada C; Chow JS [10](Figure 1).
Figure 1:
Studies show that pregnancy after bladder augmentation is relatively rare, with few cases reported in the literature. The following case report describes a successful indication for cesarean section via fundal incision in a patient with bladder augmentation due to a history of myelomeningocele.
A 27-year-old Brazilian woman on her third pregnancy with a history of two early miscarriages that did not require uterine curettage underwent a scheduled cesarean section at 39 weeks of gestational age due to maternal comorbidities. She was diagnosed with gestational diabetes, which was managed with diet. This pregnant woman with a uterine height consistent with intrauterine growth restriction was admitted and her obstetric ultrasound revealed a fetus classified as small for gestational age, with an estimated fetal weight of 2,321 grams, falling between the 3rd and 10th percentiles. She also had a known history of neurogenic bladder requiring intermittent catheterization every 3 hours secondary to myelomeningocele, a condition diagnosed and treated at birth, with no motor sequelae. Due to a neurogenic bladder and recurrent urinary tract infections, she underwent bladder augmentation with intestinal tissue at the age of 11 which led to better bladder control and reduced hospitalizations for pyelonephritis. During pregnancy, she required treatment for both outpatient cystitis and inpatient episodes of pyelonephritis. She received prophylaxis for urinary tract infections with nitrofurantoin until 36 weeks of pregnancy. She had allergies to ceftriaxone, benzathine penicillin, and vancomycin.
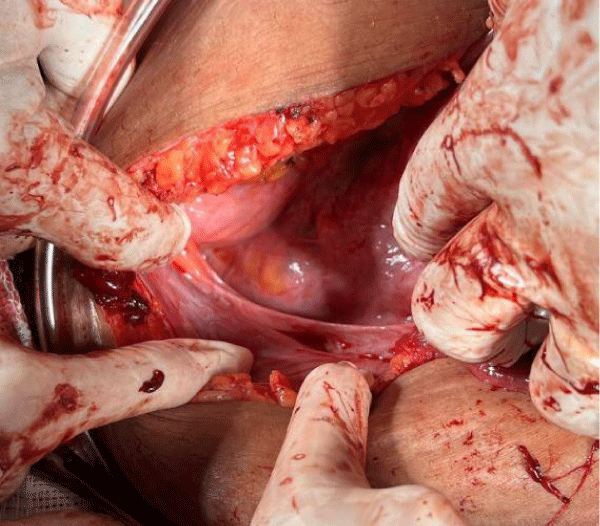
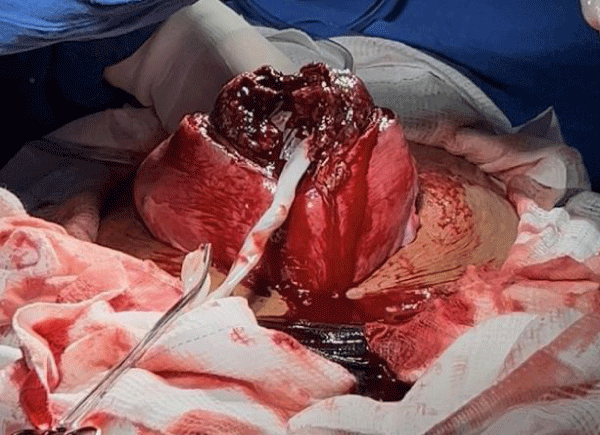
During the cesarean section, the abdominal cavity was accessed via a midline infra umbilical incision. An augmented bladder (neobladder) was identified intraoperatively without alterations (Figure 2).
Figure 2: Intact neobladder.
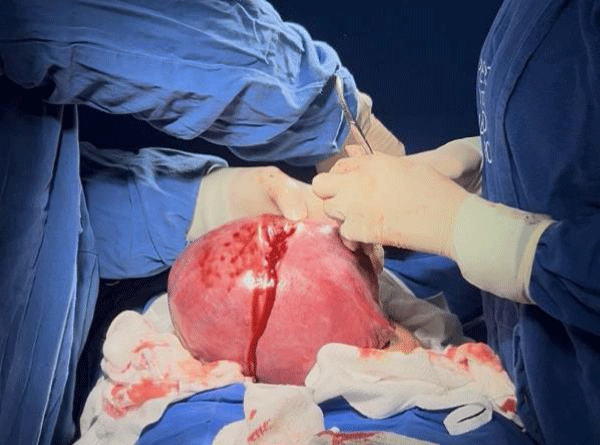
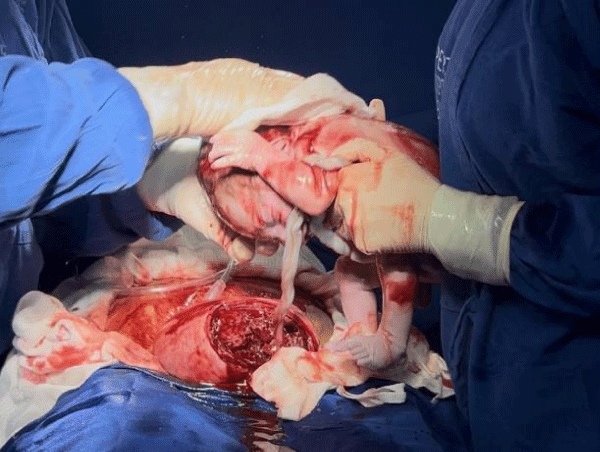
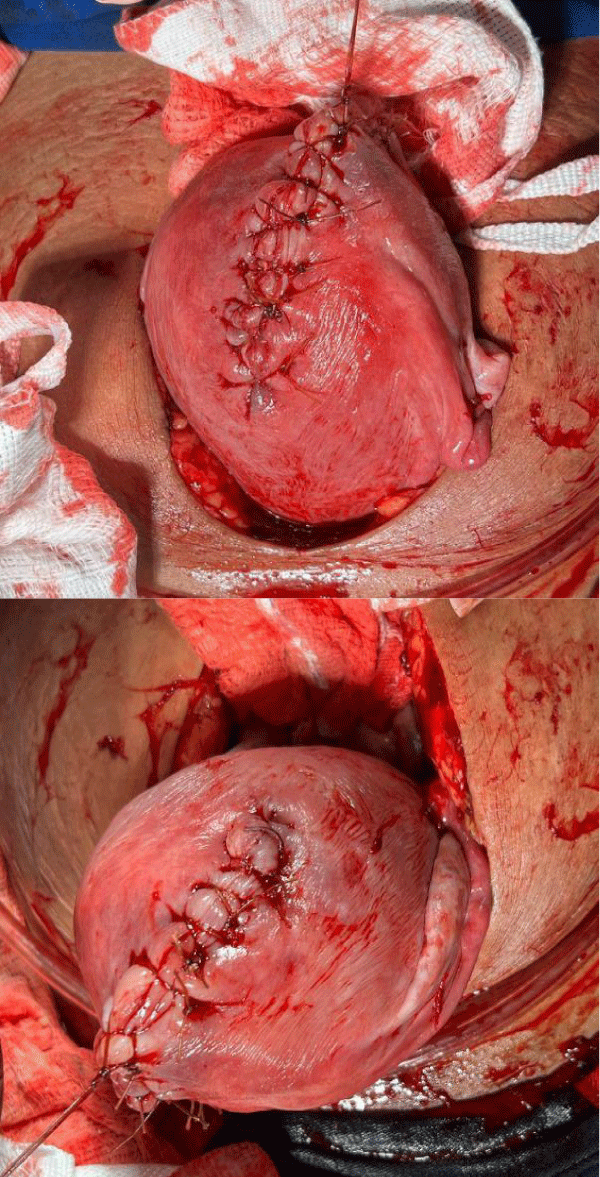
A fundal hysterotomy was chosen for fetal extraction to preserve the neobladder, with no complications. A male newborn was delivered, weighing 2,488 g, with Apgar scores of 7 and 8 (Figures 3-6).
Figure 3: Fundal hysterotomy.
Figure 4: Figure 4
Figure 5: Exposed placent.
Figure 6: Repair of the fundus.
Cystoplasty
The first report on performing a cystoplasty in a patient with a neurogenic bladder was published in 1955.
Reconstruction of the bladder using segments of the bowel is primarily performed to manage urinary frequency, incontinence, and poor bladder compliance. Correia C, Pardal C, Igreja J [11].
Augmentation cystoplasty is a surgical procedure that uses segments of the bowel to increase bladder capacity, particularly in women who lack adequate bladder function or detrusor compliance. The majority of women undergo ileocystoplasty but colocystoplasty can also be done. The common indications for augmentation cystoplasty were neurogenic bladder and decreased compliance, undiversion, exstrophy, contracted bladder, and interstitial cystitis. Correia C, Pardal C, Igreja J [11].
Premature birth, urinary tract infection, and urinary and intestinal obstruction were described in the literature. In addition, complications such as disruption of the reconstruction, impaired renal function, urinary retention, and vesicoureteral reflux may occur. Vordermark JS [2,12-15].
Elective cesarean section is advised for women who had their bladder neck, urethra, or artificial urinary sphincter reconstructed.
Clinical implications
This article highlights the importance of anticipating complications, planning elective delivery when possible, and making patient-informed choices. Obstetricians caring for women with complex urological or neurologic conditions need to:
- Carefully assess past surgical history and current anatomy.
- Coordinate care with urologists and neurologists.
- Counsel patients regarding risks of prolapse, incontinence, and surgical complications.
The indication for vaginal delivery should be carefully evaluated, as the underlying condition may affect the onset and coordination of uterine contractions, in addition to the risk of birth canal trauma, including vaginal, cervical, and bladder injuries, which may be difficult to repair. The unpredictability of the onset of labor and the availability of a multidisciplinary team must be considered.
Rather than dogmatically favoring one delivery method, this article promotes individualized care based on patient anatomy, surgical history, functional capabilities, and patient preference. It is a strong call for nuanced, interdisciplinary, and empathetic obstetric planning in a historically underserved patient population.
Ethical considerations
Patient´s consent was formally obtained. The research project was submitted for review by the Research Ethics Committee of the Leonor Mendes de Barros Maternity Hospital to ensure compliance with the guidelines and regulations governing research involving human subjects. Informed Consent Forms (ICFs) were duly obtained and signed by all participants, ensuring adherence to the ethical standards of clinical research. The project received timely approval under CAAE: 89037725.7.0000.0063. All procedures involving this patient were conducted in accordance with the ethical standards of the institutional committee.
- Ruan J, Zhang L, Duan MF, Luo DY. Pregnancy and delivery after augmentation cystoplasty: A case report and review of literature. World J Clin Cases 2022; 10(13): 4177-4184. Available from: https://doi.org/10.12998/wjcc.v10.i13.4177
- Vordermark JS. Management of pregnancy after augmentation cystoplasty. Int Urogynecol J 1991;2:36–9. Available from: https://link.springer.com/article/10.1007/BF00400042
- Shaikh A, Ahsan S, Zaidi Z. Pregnancy after augmentation cystoplasty. J Pak Med Assoc 2006;56:465–7. Available from: https://pubmed.ncbi.nlm.nih.gov/17144396/
- Hensle TW, Bingham JB, Reiley EA, Cleary-Goldman JE, Malone FD, Robinson JN. The urological care and outcome of pregnancy after urinary tract reconstruction. BJU Int 2004;93:588–90. Available from: https://doi.org/10.1111/j.1464-410x.2003.04665.x
- Taniguchi A, Kakizaki H, Murakumo M, Nonomura K, Koyanagi T. Management of pregnancy and delivery after augmentation cystoplasty. The Japanese Journal of Urology. 2002. 93(1):39-43. Available from: https://doi.org/10.5980/jpnjurol1989.93.39
- Vordermark JS, Deshon GE, Agee RE. Management of pregnancy after major urinary reconstruction. Obstet Gynecol 1990;75:564–7. Available from: https://pubmed.ncbi.nlm.nih.gov/2406671/
- Hill DE, Kramer SA. Management of Pregnancy after Augmentation Cystoplasty. The Journal of Urology, 1990; 144(2): 457–459. Available from: https://doi.org/10.1016/s0022-5347(17)39488-0
- Greenwell TJ, Venn SN, Creighton S, Leaver RB, Woodhouse CR. Pregnancy after lower urinary tract reconstruction for congenital abnormalities. BJU Int 2003;92:773–7. Available from: https://doi.org/10.1046/j.1464-410x.2003.04465.x
- Kapoor D, Chipde SS, Agrawal S, Chipde S, Kapoor R. Delivery after augmentation cystoplasty: implications and precautions. J Nat Sci Biol Med 2014;5:206–9. Available from: https://doi.org/10.4103/0976-9668.127334
- Breen M, Phelps A, Estrada C, Chow JS. The role of imaging in pediatric bladder augmentation. Pediatric Radiology. 2015; 45 (10): 1440-1447. Available from: https://doi.org/10.1007/s00247-015-3349-1
- Correia C, Pardal C, Igreja J. Management of pregnancy after augmentation cystoplasty. BMJ Case Rep. 2015:bcr2015209304. Available from: https://doi.org/10.1136/bcr-2015-209304
- Greenwell TJ, Venn SN, Creighton S, Leaver RB, Woodhouse CRJ. After cystoplasty the patient usually must empty the neobladder by intermittent self-catheterization. BJU Int 2003;92:773–7.
- Cheng PJ, Myers JB. Augmentation cystoplasty in the patient with neurogenic bladder. World J Urol. 2020; 38(12):3035-3046. Available from: https://doi.org/10.1007/s00345-019-02919-z
- Hansen EL, Hvistendahl GM, Rawashdeh YF, Olsen LH. Promising long-term outcome of bladder autoaugmentation in children with neurogenic bladder dysfunction. J Urol. 2013;190(5):1869-75.Available from: https://doi.org/10.1016/j.juro.2013.05.035
- Çetinel B, Kocjancic E, Demirda? Ç. Augmentation cystoplasty in neurogenic bladder. Investig Clin Urol. 2016;57(5):316-23. Available from: https://doi.org/10.4111/icu.2016.57.5.316