More Information
Submitted: December 05, 2025 | Accepted: December 15, 2025 | Published: December 16, 2025
Citation: Turker Y, Erdem MY, Cihan YB. Diffuse Dural Thickening and Contrast Enhancement. Arch Case Rep. 2025; 9(12): 407-408. Available from:
https://dx.doi.org/10.29328/journal.acr.1001178
DOI: 10.29328/journal.acr.1001178
Copyright license: © 2025 Turker Y, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Dural metastasis; Prostate cancer; Facial paralysis; Magnetic resonance imaging; Case report
Diffuse Dural Thickening and Contrast Enhancement
Yusuf Turker, Mehmet Yasin Erdem and Yasemin Benderli Cihan*
Department of Radiation Oncology, Kayseri City Education and Research Hospital, Kayseri, Turkey
*Corresponding author: Yasemin Benderli Cihan, MD, Department of Radiation Oncology, Kayseri City Education and Research Hospital, Seker District, Muhsinyazıcıoğlu Boulevard, No:77, 38080, Kocasinan/Kayseri, Turkey, Email: [email protected]
Dural metastasis is a rare sign of advanced cancers, most often linked to breast, lung, and prostate cancers. With better survival rates in metastatic prostate cancer due to improvements in systemic treatment, unusual patterns like dural involvement are becoming more common. We present an unusual case of widespread dural metastasis from prostate adenocarcinoma that resulted in facial paralysis. A 69-year-old man with metastatic prostate cancer and extensive bone involvement came in with a headache and one-sided facial paralysis. A cranial MRI showed thickening of the dura and contrast enhancement affecting all dural surfaces. The patient received corticosteroids and palliative whole-brain radiotherapy, but he passed away from pneumonia three weeks later. This case emphasizes the need to consider dural metastasis in cancer patients who show unusual neurological symptoms. Early detection with cranial MRI is essential, and radiotherapy is an important option for palliative care. Reporting such rare cases helps improve awareness and guides clinical decisions.
With the emergence of new treatment modalities, the expected survival of patients with metastatic prostate cancer has improved. Consequently, diagnoses that were previously rare—such as dural metastasis (DM)—are now being encountered more frequently, making their management increasingly important. The most common primary tumors associated with DM are prostate, breast, and lung carcinomas [1]. Studies analyzing DM have shown that breast cancer (16% - 34%) and prostate cancer (17% - 19.5%) are the leading causes. Among male patients, approximately 43% of dural metastasis cases originate from prostate adenocarcinoma [2].
DM may develop through direct invasion of calvarial metastases, invasion of parenchymal or leptomeningeal metastases into the dura, or via hematogenous spread. The most common mechanism is direct extension from calvarial metastases [3]. Patients with DM may present with various neurological symptoms, including seizures, paralysis, speech disturbances, and subdural hematomas due to increased intracranial pressure [4]. In this report, we present a rare case of DM manifesting with facial paralysis.
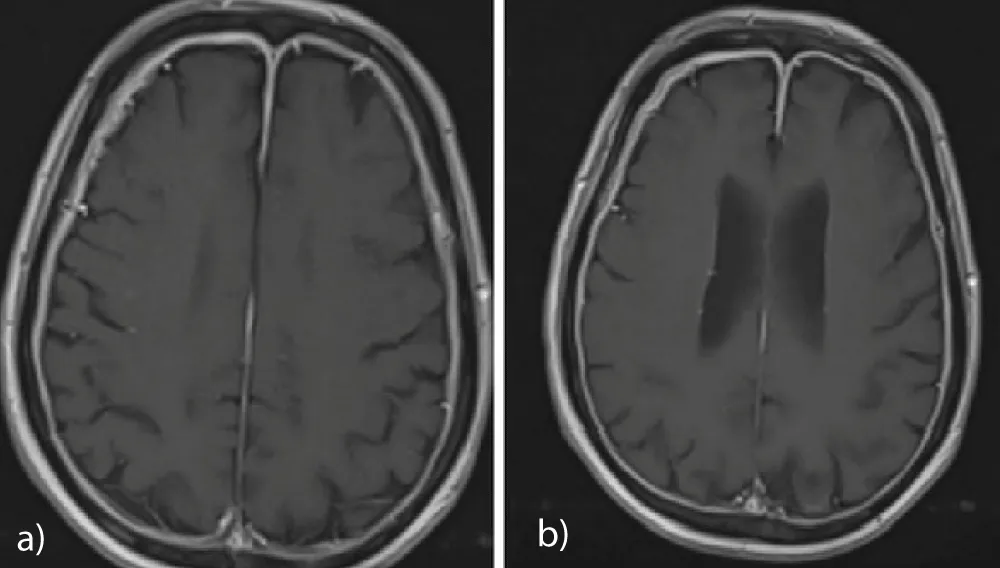
The patient was a 69-year-old man who had been treated with goserelin, abiraterone, and lutetium-177 due to metastatic prostate cancer with extensive bone involvement. He had been evaluated as having stable disease and was followed accordingly. His medical history included hypertension and aortic stenosis. The patient presented to the neurology outpatient clinic with complaints of headache and facial paralysis. Cranial MRI revealed diffuse thickening and contrast enhancement of all dural surfaces on T1-weighted images, and he was subsequently referred to our clinic (Figure 1a,b). On physical examination, his general condition was moderate; he was conscious, oriented, semi-cooperative, and bed-mobile, with a Glasgow Coma Score of 14-15. Neurological examination revealed bilateral muscle strength of 4+/5 and left-sided facial paralysis. Anti-edema treatment with dexamethasone was initiated. Whole-brain radiotherapy was delivered using a LINAC device with 6 MV photon energy at a dose of 8 Gy in a single palliative fraction. Three weeks after radiotherapy, the patient was reported to have died due to pneumonia.
Figure 1: a,b: Diffuse dural thickening and contrast enhancement on T1-weighted cranial MRI.
A multidisciplinary approach is essential in the management of DM. Treatment options include surgery, radiotherapy, systemic therapy, or combinations of these modalities. Selection of the appropriate treatment method should be based on the patient’s overall condition and the extent of metastatic disease. The average survival time is approximately 9–10 months. Although there is no standardized treatment approach for DM, surgery and radiotherapy have been reported to be effective in many cases. Surgical resection may be beneficial when the lesion is resectable and systemic disease is under control [5].
In conclusion, dural metastases may present with different clinical symptoms depending on tumor burden and localization. DM should be considered in cancer patients presenting with facial paralysis. Cranial MRI is essential for diagnosis. Radiotherapy plays an important role in treatment and has been shown to improve prognosis. We believe that this case contributes to the literature due to its unusual presentation with diffuse dural metastasis in the absence of cranial or intradural metastatic lesions.
- Rios-Vicil CI, De Jesus O. Prostate adenocarcinoma dural metastasis mimicking a subacute subdural hematoma. Surgical Neurology International. 2025;16:60. Available from: https://surgicalneurologyint.com/surgicalint-articles/prostate-adenocarcinoma-dural-metastasis-mimicking-a-subacute-subdural-hematoma/
- Kokot K, Dzierzanowski J, Krakowiak M, Fercho J, Yuser R, Kosel L, et al. Dural metastasis of prostate carcinoma mimicking intracranial hematoma: a case report and literature review. Journal of Surgical Case Reports. 2024;2024(2):rjae014. Available from: https://academic.oup.com/jscr/article/2024/2/rjae014/7600403
- Rios-Vicil CI, De Jesus O. Prostate adenocarcinoma dural metastasis mimicking a subacute subdural hematoma. Surgical Neurology International. 2025 Feb 21;16:60. Available from: https://surgicalneurologyint.com/surgicalint-articles/prostate-adenocarcinoma-dural-metastasis-mimicking-a-subacute-subdural-hematoma/
- Zhang S, Xu Y, Hui X, Yang F, Hu Y, Shao J, et al. Improvement in prediction of prostate cancer prognosis with somatic mutational signatures. Journal of Cancer. 2017 Sep 15;8(16):3261–3267. Available from: https://www.jcancer.org/v08p3261.htm
- Kobayashi M, Sasagawa Y, Nakada S, Kohda Y, Nakada M. Dural metastasis from prostate carcinoma mimicking tuberculum sellae meningioma: a case report. Surgical Neurology International. 2022;13:407. Available from: https://surgicalneurologyint.com/surgicalint-articles/dural-metastasis-from-prostate-carcinoma-mimicking-tuberculum-sellae-meningioma/