More Information
Submitted: March 06, 2024 | Approved: March 25, 2024 | Published: March 26, 2024
How to cite this article: García AC, Mateo SG, Bennike MSG, García BA, Álvarez MTG, et al. Navigating Diagnostic Dilemmas in Subacute Subdural Hemorrhage: A Case Report. Arch Case Rep. 2024; 8: 039-041.
DOI: 10.29328/journal.acr.1001091
Copyright License: © 2024 García AC, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Navigating Diagnostic Dilemmas in Subacute Subdural Hemorrhage: A Case Report
Alicia Cárdenas García1*, Sara García Mateo2, María Sol González Bennike3, Berta Alonso García1, María Teresa Gómez Álvarez4, Francisco de Borja Hernández Moreno4 and Clara Ponce Aceituno3
1Third-year Medical Resident, Villalba General Hospital, Madrid, Spain
2Second-year Medical Resident, Villalba General Hospital, Madrid, Spain
3First-year Medical Resident, Villalba General Hospital, Madrid, Spain
4Specialist Doctor, Villalba General Hospital, Madrid, Spain
*Address for Correspondence: Alicia Cárdenas García, Third-year Medical Resident, Villalba General Hospital, Madrid, Spain, Email: [email protected]
In this case report a 64-year-old male patient with recent past medical history of head injury complicated by zygomatic arc fracture and mild subarachnoid hemorrhage is studied. He had been presented to the Emergency Department because of progressive neurological symptoms and neurological deficits in the physical examination that could have been indicating subcacute subdural hemorrhage. However, the patient was reluctant to undergo diagnostic imaging due to concerns about radiation exposure. After several explanations, a CT scan was done, which revealed a bilateral subacute subdural hematoma. Neurosurgical management was initiated and intravenous corticosteroid therapy was administered to reduce local edema. The challenge of this case is based on the subtlety of symptoms that might cause patients to delay seeking medical attention. Additionally, patient reluctance to undergo diagnostic tests can complicate management, emphasizing the importance of patient education and therapeutic alliance. Multidisciplinary management involving Neurology and Neurosurgery is crucial for optimal patient care in such cases. This report underscores the significance of effective communication and collaborative decision-making between healthcare providers and patients to ensure timely and appropriate management of complex medical conditions.
Subdural hemorrhage is a condition caused by superficial bleeding of the brain, beneath the dura mater. This condition could be acute, subacute, and chronic and usually is caused by severe high-impact injury. Subacute subdural hemorrhage is the gradual bleeding in the subdural space that happens in 4 days - 21 days after head traumatism. Its diagnosis is a challenge due to its subtle and evolving symptoms, often leading to delayed medical intervention [1,2].
This case report illustrates the clinical course of a 64-year-old male with a history of head injury, emphasizing the complexities encountered in diagnosis and management. Head injuries, particularly those involving fractures and hemorrhage, can result in various neurological sequelae, highlighting the critical need for vigilant monitoring and timely intervention. Despite advancements in medical imaging and diagnostic techniques, patients’ reluctance to undergo certain procedures can further complicate diagnosis and treatment. Understanding the clinical presentation, diagnostic approach, and management strategies for subacute subdural hemorrhage is essential for healthcare providers to deliver optimal care and improve patient outcomes [3-5].
The importance of this study lies in shedding light on the challenges faced in diagnosing and managing subacute subdural hemorrhage, particularly in patients with pre-existing neurological conditions or those exhibiting reluctance towards medical interventions.
This study contributes to the existing literature on subacute subdural hemorrhage and reinforces the importance of early recognition, prompt intervention, and patient-centered care in optimizing outcomes for individuals affected by this condition [6-9].
− Year: 2023.
− Location: Emergency Department, Villalba General Hospital, Madrid, Spain [10,11].
− Objective: Illustrating the diagnostic challenges and management complexities associated with subacute subdural hemorrhage.
− Procedure: Comprehensive clinical examination, inclu-ding neurological assessment and diagnostic imaging
− Importance: Highlights the importance of timely diagnosis and multidisciplinary management in opti-mizing outcomes for patients with subacute subdural hemorrhage.
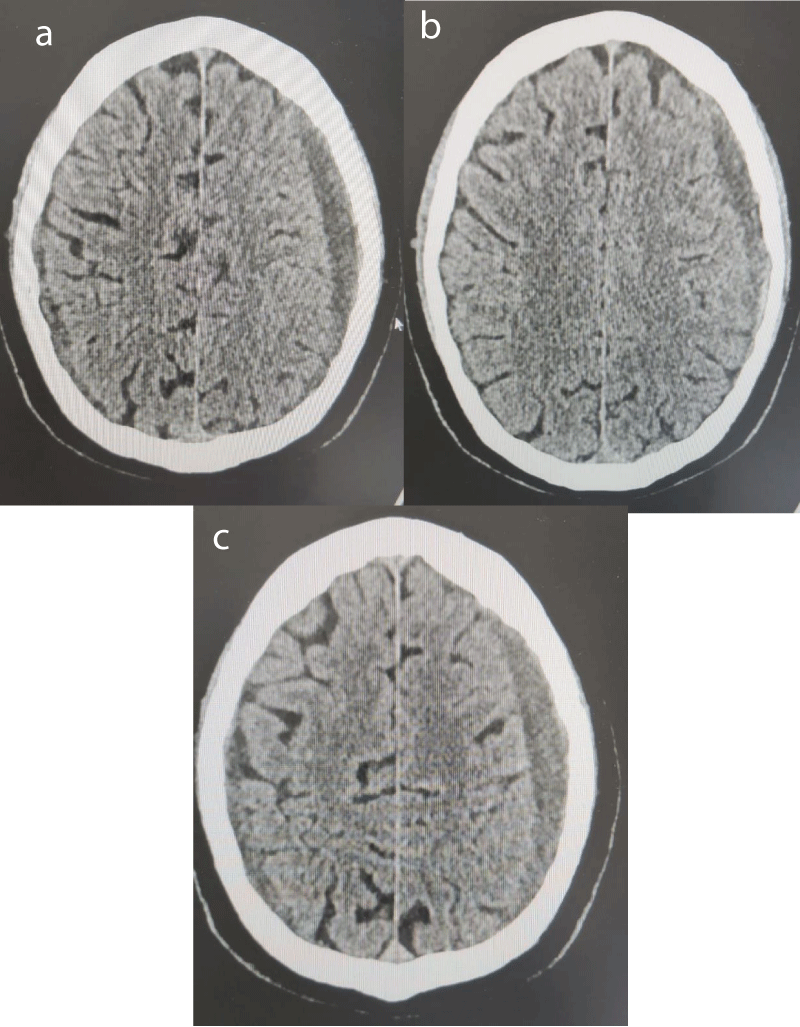
Figure 1: a) Blood test: No notable values are seen in the analysis. b) CT-scan: subacute bilateral subdural hematomas of 22 and 17 mm respectively with frontal extension. (a,b,c).
A 64-year-old male, without active medical treatment, as past medical history is remarkable a head injury three months ago that required hospitalization for five days due to a zygomatic arch fracture and mild subarachnoid hemorrhage. The patient came to the Emergency Department complaining of progressive difficulty in walking, slowness, difficulty in starting to walk, and weakness that has been worsening in the last month.
Clinical examination
Blood pressure: 126/83 mmHg, Heart rate: 76 bpm, Temperature: 36.2 ºC, Saturation 97%, Glasgow 15/15. Conscious and alert, oriented in time and space. Well hydrated, nourished, and perfused.
a) Cardiac auscultation: Rhythmic, no auscultation murmurs or extra tones.
b) Pulmonary auscultation: Normal vesicular murmur.
c) Abdomen: Soft and depressible, not painful on palpa-tion. I do not feel masses or mealies. No signs of peritoneal irritation. Negative dorsal cust-percussion.
d) Lower extremities: No edema, peripheral pulses preserved, no signs of deep vein thrombosis.
e) Neurological examination: bradylalia, increased reflexes on the left side, an increase of the base of support walking, decreased arm movements on the right side, and Tandem lateralization to the right side [12,13].
Evolution
After anamnesis and physical examination, we requested blood tests and a CT scan to study a differential diagnosis between space-occupying lesions, intracranial hypertension, or intracranial hemorrhage.
The patient is very reluctant to realize the CT scan, explaining the fear of the iatrogenic radiation associated with the test [14,15]. The need for the imaging testing is explained to the patient and his family, due to the importance of the correct management of the case, and assessing the risk-benefit [16].
Objective tests and procedures
Due to the findings, Neurosurgical evaluation is requested and intravenous corticosteroid therapy is started to reduce local edema (Figure 1a-c).
Subacute subdural hemorrhage is a complication that is difficult to diagnose, because the symptoms can be latent over time and cannot be clinically expressive, so patients may take a long time to consult or even if they do so and not receive the necessary care.
In this case, there was an added difficulty, the patient’s suspension. He was very reticent to do the tests and given the involvement of the hemorrhage in the frontal area, bradylalia and bradypsychia made its management complicated. Part of the refusal was his conviction and part was due to not being in his full faculties because of hemorrhage. The case underscores the diagnostic challenges posed by subacute subdural hemorrhage, emphasizing the importance of prompt evaluation and multidisciplinary collaboration for optimal patient care [17].
Furthermore, I would like to add the importance of the therapeutic alliance with the patient, the need to not give up on their refusal when we, as facultatives, consider a beneficial medical act, the value of explaining to the patient and their family correctly the procedure for making collective decisions as a team (not giving up by extending voluntary discharge) and the interesting aspects of multidisciplinary management with different specialists (in this case with Neurology and Neurosurgery).
In conclusion, navigating cases of subacute subdural hemorrhage, clinicians must prioritize thorough assessment and effective communication to address patient concerns and facilitate timely intervention. Similar findings by other medical practitioners further highlight the significance of this condition and the need for standardized protocols to ensure consistent diagnosis and management across healthcare settings.
Declaration
I, Alicia Cárdenas García, declare that I have no conflict of interests pertaining to the study described herein. I affirm that I have not received any financial compensation, including payments or private financial support, for conducting or contributing to this study. As the main author of this research, I assert that my involvement in this study was motivated solely by scientific inquiry and the pursuit of knowledge. Furthermore, I acknowledge the contributions of my colleagues, (Sara García Mateo, María Sol González Bennike, Berta Alonso García, María Teresa Gómez Álvarez, Francisco de Borja Hernández Moreno and Clara Ponce Aceituno), who participated in this research endeavor. I hereby disclose that there are no competing interests that could potentially bias the interpretation or dissemination of the findings presented in this study.
I, Alicia Cárdenas García, hereby declare that the patient involved in the case study described herein has provided explicit consent for the study and documentation of their medical condition. The patient has been informed about the purpose and scope of the study, as well as the potential implications of their participation. They have voluntarily agreed to participate and have granted permission for the use of relevant medical information for academic and research purposes. Confidentiality measures have been strictly adhered to throughout the study, and all efforts have been made to ensure the anonymity of the patient. I affirm that this declaration is made in accordance with ethical guidelines and standards governing medical research and patient confidentiality.
- Papa L, Goldberg SA. Head trauma. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier. 2023: chap 33.
- Stippler M, Mahavadi A. Craniocerebral trauma. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier. 2022; chap 62.
- Kim YW, Kim YS, Kim SW. Subacute subdural hematoma: clinical characteristics and predictive factors for surgical treatment. Journal of Korean Neurosurgical Society. 2021; 64(5):713–720.
- Foo D, Rossier AB, Goumas C. Subacute subdural haematoma: correlation of clinical features with neuroimaging findings. British Journal of Neurosurgery. 2019; 7(2):131–138.
- Lee JH, Park JY, Park JW. Clinical analysis of spontaneous subacute subdural hematoma. Journal of Korean Neurosurgical Society. 2018; 61(2):179–187.
- Grzonka P, Ahmed A, Richter HP. Spontaneous chronic subdural haematoma with extended clinical symptoms. British Journal of Neurosurgery. 2016; 10(4):325–328.
- Okano A, Oya S. A Case of Subacute Subdural Hematoma Mimicking a Benign Cystic Lesion. World Neurosurgery. 2020; 7(2):201–205.
- Mendelow AD, Gregson BA. Early surgery versus initial conservative treatment in patients with traumatic intracerebral hemorrhage (STITCH[Trauma]): the results of a randomized trial. Lancet Neurology. 2015; 15(2):137–143.
- Sun H, Xie Y, Yan J. Clinical features and risk factors of chronic subdural hematoma: comparison of patients with single and recurrent episodes of chronic subdural hematoma. World Neurosurgery. 2019; 5(3):429–435.
- Ko JK, Lee JH, Choi BJ. Risk factors of acute and chronic subdural hematoma: a retrospective study. Clinical Neurology and Neurosurgery. 2017; 9(4):124–130.
- Sim JH, Shin JH, Kang JH. Risk factors and outcomes in patients with spontaneous acute subdural hematoma. Journal of Korean Neurosurgical Society. 2018; 61(5):632–639.
- Kwon HY, Kim JH, Kim SH. Surgical outcomes and prognostic factors of subacute subdural hematoma in older patients. World Neurosurgery. 2020; 15(6):180–185.
- Lee JH, Park JW. Analysis of predictors of prognosis and long-term outcomes of chronic subdural hematoma management using nationwide databases. Neurosurgery. 2019; 16(4):1065–1071.
- Park JY, Lee JH. A retrospective analysis of risk factors and clinical outcomes in patients with subdural hematoma. Journal of Korean Neurosurgical Society. 2017; 60(3):355–362.
- Han SR, Kim HJ. Predictive factors for recurrence and clinical outcomes in patients with chronic subdural hematoma. Journal of Neurological Surgery. 2016; 17(1):81–87.
- Wang C, Guo H, Xue Z. Clinical characteristics and risk factors for recurrence of chronic subdural hematoma: a retrospective analysis of 398 cases. PLoS ONE. 2018; 9(3):e0224585.
- Wu C, Yan S, Fu K. Clinical analysis of 94 cases of subacute subdural hematoma. Zhonghua Yi Xue Za Zhi. 2020; 22(8):781–785.