More Information
Submitted: March 06, 2024 | Approved: March 25, 2024 | Published: March 26, 2024
How to cite this article: Alfieri A, Rapanà A, Caranci F. Endoscopic Endonasal total Removal of a Suprasellar, Preinfundibular Retro Chiasmatic Craniopharyngioma: A Surgical Case Report. Arch Case Rep. 2024; 8: 036-038.
DOI: 10.29328/journal.acr.1001090
Copyright License: © 2024 Alfieri A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Endonasal transsphenoidal approach; Craniopharyngioma; Suprasellar craniopharyngioma; Extended transsphenoidal approach
Endoscopic Endonasal total Removal of a Suprasellar, Preinfundibular Retro Chiasmatic Craniopharyngioma: A Surgical Case Report
Alessandra Alfieri1, Armando Rapanà2 and Ferdinando Caranci3*
1Department of Neurosurgery, “S. Anna e S. Sebastiano” Hospital, Caserta, Italy
2Department of Neurosurgery, “S. Giuseppe Moscati” Hospital, Avellino, Italy
3Department of Precision Medicine, “Luigi Vanvitelli” University of Campania,
Naples, Italy
*Address for Correspondence: Ferdinando Caranci, MD, Full Professor of Neuroradiology, Department of Precision Medicine, “Luigi Vanvitell” University of Campania, Naples, Italy, Email: [email protected]
Craniopharyngiomas are benign tumors (WHO Grade I), seen in children and adults. Because of their location, they can require challenging clinical and surgical management. In fact, often, because of the presence of calcifications, of a capsule very strongly adherent to neurovascular structures, of the relationship with hypophysis, pituitary stalk, chiasm, carotids, the circle of Willis, basilar artery, and third ventricle, risk of mortality and morbidity is still mandatory. Various surgical techniques have been proposed: transcranial, transsphenoidal, and supraorbital approaches for surgical resection and treatment of craniopharyngiomas. Still, there is no common consent, but often the endonasal transsphenoidal extended procedures are considered the gold standard in many cases. We present a surgical technique of a case of complete surgical removal of an infundibular and retro chiasmatic craniopharyngioma, via an endoscopic endonasal transphenoidal transplanum approach.
Craniopharyngiomas are rare epithelial tumors. They account for 2.5% of all primary intracranial neoplasms and originate from remnants of Rathke’s pouch, a small sac-like structure that is present in the developing fetus and later forms part of the pituitary gland normally, a small piece of Rathke’s pouch persists after birth. These tumors typically arise in the suprasellar region of the brain and affect the hypothalamus, the optic chiasm, the cranial nerves, the third ventricle, and the intracranial vessels. Very rarely they can develop exclusively infrasellar into the sphenoid sinus [1-3].
The most common location of infrasellar craniopharyngiomas is the sphenoid sinus, either alone or combined with other sites such as the nasopharynx, sella turcica, suprasella, ethmoid sinuses, or maxillary sinus. Craniopharyngioma can happen at any age, but it occurs most often with a bimodal age distribution in children and older adults. With a first peak occurring in childhood and early adolescence, predominately at age 5-10 years, and a second peak at age 40-60 years. These tumors occur equally in men and women. Symptoms include changes in vision over time, fatigue, headaches, and urinating more often. As they are slow-growing tumors, they are usually diagnosed late, when the patient develops symptoms of compression. Although benign, they are difficult to treat surgically due to their location and close relationships with critical neurovascular structures. The first step in treatment is surgery. When a complete removal is not achieved, radiation therapy is done, with a high long-term cure rate [4]. Still, there is no general agreement on the best surgical approach, transcranial or endonasal [5-15]. We present a case of complete surgical removal of an infundibular and retro chiasmatic craniopharyngioma, via an endoscopic endonasal transsphenoidal transplant approach.
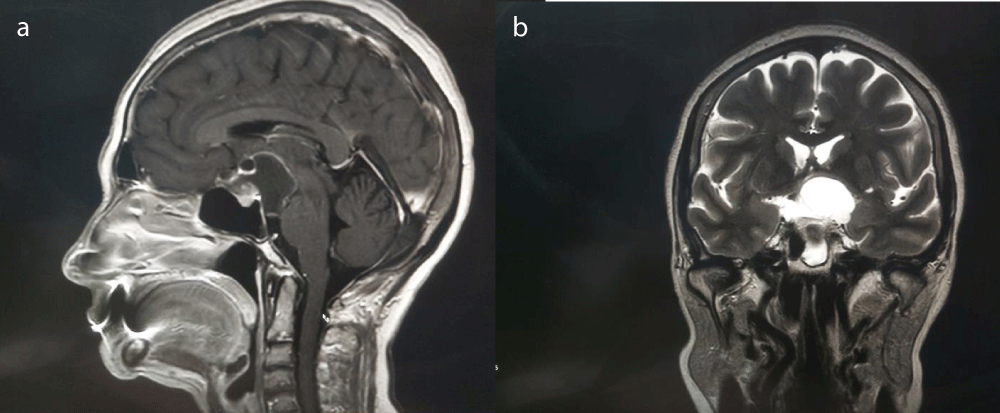
In 2015 in the Department of Neurosurgery of the S. Anna and S. Sebastiano Hospital of Caserta, Italy, a 63-year-old woman was referred with bitemporal hemianopia and hypocorticoadrenalism. A CT scan showed a suprasellar mass with calcifications. MRI showed a suprasellar lesion with intracranial and retrochiasmatic extension, heterogeneous texture, and a combination of solid, cystic, and calcified components. Coronal T2-weighted contrast-enhanced images show the presence of a large mass, peripherally enhancing, occupying the suprasellar region and extending behind the dorsum; small enhancing nodular solid components are noted in the anterior part of the lesion. The optic chiasm was displaced upwards while the pituitary gland was separated from the mass (Figure 1a,b). The preoperative pituitary function assessment showed hypocorticoadrenalism.
Figure 1: a) Pre-operative Sagittal T1 weighted contrast-enhanced MRI.b) Preoperative Coronal T2 weighted MRI.
The patient was operated on using an extended endonasal endoscopic transphenoidal tranplanum approach. A two-nostril procedure with a robotic endoscopic pneumatic holder was performed. The planum sphenoidale was drilled out and the dura was opened. A yellow encapsulated granulated tissue was exposed. The craniopharyngioma displaced upward the chiasm. With the endoscope secured to a robotic holder and a two-four-hand procedure, the tumor was completely dissected from the neurovascular structures and removed. Helpfully, was possible the dissection and total removal of the tumor and of the capsule (Video). An intrasellar packing with abdominal autologous fat, neuropathy, and fibrin glue was done. The sella was reconstructed with autologous septal bone.
The histologic pattern showed an adamantinomatous craniopharyngioma.
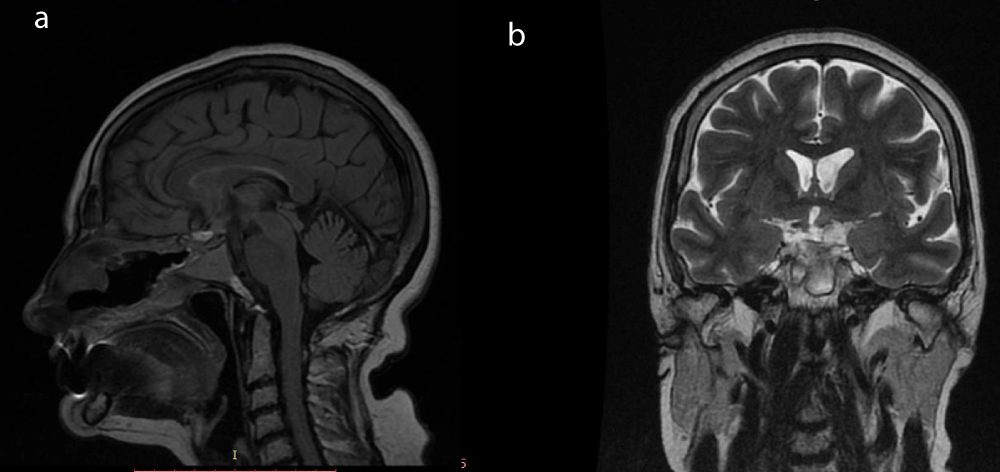
After the operation, the visual deficit improved and the patient was discharged 5 days after surgery without any complications. The post-operative pituitary function was unchanged and no post-operative CSF leak occurred. Postoperative MRI showed complete removal of the craniopharyngioma. After a nine-year follow-up, the patient has no recurrence (Figure 2a,b).
Figure 2: a) Post-operative sagittal MRI. b) Post-operative coronal MRI.
Surgical video description. A yellow encapsulated granular tissue with calcifications was found. The chiasm, the stalk, and the pituitary gland were nicely seen and preserved, as well as the circle of Willis.
First, the suprasellar preinfundibular part and then the retro chiasmatic lesion was removed. The entire lesion and capsule were removed under direct endoscopic view of the neurovascular structures. A dissection of the capsule was particularly favorable because of the lack of strong adhesion to the neurovascular structures.
Adamantinomatous craniopharyngiomas (ACP) occur mainly in pediatrics, but can also occur in adults. They have a solid and a cystic part.
Craniopharyngiomas can behave malignantly due to their location and close relationship to vital neural and vascular structures. Gross total excision does not seem to change their behavior in terms of conservative treatment, so total excision is recommended when possible. In addition, there is much controversy about the preferred surgical approach for these tumors. Nowadays, the endoscopic, endonasal, extended approach is considered the treatment of choice [2,5-8]. Recent studies have suggested that a supraorbital “keyhole” approach may be more efficacious for the resection of several skull-base tumor types [9]. Webb, et al. compared the transcranial approach and the transsphenoidal approaches and concluded that endonasal approaches result in a lower incidence of tumor recurrence, improved visual outcomes, and reduced incidence of postoperative seizures, but CSF leak is still more frequent in the transsphenoidal approach [10]. Compared to the established transcranial approaches (pterional, sub-frontal, presigmoid), endoscopic endonasal surgery allows direct infra chiasmatic exposure without the need to manipulate critical neurovascular structures to gain access to the tumor [10-15]. In addition, injury to the adjacent hypothalamus, infundibulum, pituitary gland, optic tract, or vasculature can have devastating consequences, including hypothalamic obesity, autonomic dysregulation, panhypopituitarism, blindness, and severe strokes. A total resection is not always possible and often capsule and calcification removal can lead to increased morbidity and mortality [3].
In this case, the chiasm was displaced upward by the lesion. This aspect was an advantage in preserving optical chiasm integrity. A complete excision of the tumor was possible, with the chiasm, infundibulum, pituitary gland, and pituitary stalk, and the circle of Willis clearly visible. A favorable ratio of the capsule, which was easily detached from all these vital structures, led us to complete removal. Not always the capsule is easily detachable, but an attempt should be always made, with the goal of a complete removal without high morbidity.
Surgical treatment of craniopharyngioma is still demanding. There is still no consensus on the best surgical treatment, even if many authors prefer the endoscopic endonasal extended procedures because of a direct anatomic approach to neurovascular structures and a reduced morbidity to brain structures [8-15]. Even if very challenging, we believe that an attempt to remove the capsule should be always made, even if a strong relationship with vital structures can force the surgeon to leave it inside. The first operation is always the best opportunity to cure the patient. The goal is to obtain the best result with a reduced surgical risk. Correct pre-operative planning with a meticulous study of the anatomy is mandatory to improve the results. There is no standardized treatment, but the best option is tailored for each patient, taking into account the morphology, extent, consistency, displacement, and relationship of neurovascular structures. However, after choosing preoperatively the approach, the final decision can be taken intraoperatively regarding the function of the characteristics of the tumor and the adherence of the capsule.
In the case of partial removal, complementary radiotherapy is performed [4,10.11].
- Ahsan F, Rashid H, Chapman A, Ah-See KW. Infrasellar craniopharyngioma presenting as epistaxis, excised via Denker's medial maxillectomy approach. J Laryngol Otol. 2004 Nov;118(11):895-8. doi: 10.1258/0022215042703688. PMID: 15638981.
- Magill ST, Jane JA, Prevedello DM. Editorial. Craniopharyngioma classification. J Neurosurg. 2021 Mar 5;135(5):1293-1295. doi: 10.3171/2020.8.JNS202666. PMID: 33668034.
- Almeida JP, Workewych A, Takami H, Velasquez C, Oswari S, Asha M, Bernardo A, Gentili F. Surgical Anatomy Applied to the Resection of Craniopharyngiomas: Anatomic Compartments and Surgical Classifications. World Neurosurg. 2020 Oct;142:611-625. doi: 10.1016/j.wneu.2020.05.171. PMID: 32987617.
- Schoenfeld A, Pekmezci M, Barnes MJ, Tihan T, Gupta N, Lamborn KR, Banerjee A, Mueller S, Chang S, Berger MS, Haas-Kogan D. The superiority of conservative resection and adjuvant radiation for craniopharyngiomas. J Neurooncol. 2012 May;108(1):133-9. doi: 10.1007/s11060-012-0806-7. Epub 2012 Feb 15. PMID: 22350375; PMCID: PMC3879154.
- Ruggeri AG, Cappelletti M, Giovannetti F, Priore P, Pichierri A, Delfini R. Proposal of Standardization of Closure Techniques After Endoscopic Pituitary and Skull Base Surgery Based on Postoperative Cerebrospinal Fluid Leak Risk Classification. J Craniofac Surg. 2019 Jun;30(4):1027-1032. doi: 10.1097/SCS.0000000000005540. PMID: 30908447.
- Giovannetti F, Barbera G, Priore P, Pucci R, Della Monaca M, Valentini V. Fascia Lata Harvesting: The Donor Site Closure Morbidity. J Craniofac Surg. 2019 Jun;30(4):e303-e306. doi: 10.1097/SCS.0000000000005223. PMID: 30845088.
- Giovannetti F, Mussa F, Priore P, Scagnet M, Arcovio E, Valentini V, Genitori L. Endoscopic endonasal skull base surgery in pediatric patients. A single center experience. J Craniomaxillofac Surg. 2018 Dec;46(12):2017-2021. doi: 10.1016/j.jcms.2018.09.013. Epub 2018 Sep 24. PMID: 30318327.
- Webb KL, Pruter WW, Hinkle ML, Walsh MT. Comparing Surgical Approaches for Craniopharyngioma Resection Among Adults and Children: A Meta-analysis and Systematic Review. World Neurosurg. 2023 Jul;175:e876-e896. doi: 10.1016/j.wneu.2023.04.037. Epub 2023 Apr 14. PMID: 37062335.
- Eroglu U, Shah K, Bozkurt M, Kahilogullari G, Yakar F, Dogan İ, Ozgural O, Attar A, Unlu A, Caglar S, Cohen Gadol AA, Ugur HC. Supraorbital Keyhole Approach: Lessons Learned from 106 Operative Cases. World Neurosurg. 2019 Apr;124:e667-e674. doi: 10.1016/j.wneu.2018.12.188. Epub 2019 Jan 17. PMID: 30659969.
- Müller HL. The Diagnosis and Treatment of Craniopharyngioma. Neuroendocrinology. 2020;110(9-10):753-766. doi: 10.1159/000504512. Epub 2019 Nov 4. PMID: 31678973.
- Müller HL. Craniopharyngioma. Endocr Rev. 2014 Jun;35(3):513-43. doi: 10.1210/er.2013-1115. Epub 2014 Jan 27. PMID: 24467716.
- O'steen L, Indelicato DJ. Advances in the management of craniopharyngioma. F1000Res. 2018 Oct 11;7:F1000 Faculty Rev-1632. doi: 10.12688/f1000research.15834.1. PMID: 30363774; PMCID: PMC6182675.
- Henderson F Jr, Schwartz TH. Update on management of craniopharyngiomas. J Neurooncol. 2022 Jan;156(1):97-108. doi: 10.1007/s11060-021-03906-4. Epub 2021 Nov 22. PMID: 34807341.
- Marx S, Clemens S, Schroeder HWS. The value of endoscope assistance during transcranial surgery for tuberculum sellae meningiomas. J Neurosurg. 2018 Jan;128(1):32-39. doi: 10.3171/2016.11.JNS16713. Epub 2017 Apr 7. PMID: 28387626.
- Jeswani S, Nuño M, Wu A, Bonert V, Carmichael JD, Black KL, Chu R, King W, Mamelak AN. Comparative analysis of outcomes following craniotomy and expanded endoscopic endonasal transsphenoidal resection of craniopharyngioma and related tumors: a single-institution study. J Neurosurg. 2016 Mar;124(3):627-38. doi: 10.3171/2015.3.JNS142254. Epub 2015 Sep 11. PMID: 26361276.