More Information
Submitted: October 14, 2023 | Approved: November 06, 2023 | Published: November 07, 2023
How to cite this article: Gavrilyuk VP, Severinov DA, Zubkova YA. Dermoid Cyst of the Mesentery of the Jejunum Following Appendectomy: A Clinical Case. Arch Case Rep. 2023; 7: 058-061.
DOI: 10.29328/journal.acr.1001080
Copyright License: © 2023 Gavrilyuk VP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Dermoid cyst; Appendectomy; Children; Surgery
Dermoid Cyst of the Mesentery of the Jejunum Following Appendectomy: A Clinical Case
Gavrilyuk VP1 , Severinov DA2*
, Severinov DA2* and Zubkova YA3
and Zubkova YA3
1Associate Professor, Head of the Department of Pediatric Surgery and Pediatrics,
Institute of Continuing Education, Kursk State Medical University (Kursk, Russian Federation),
Russia
2Associate Professor, Department of Pediatric Surgery and Pediatrics, Institute of
Continuing Education, Kursk State Medical University (Kursk, Russian Federation), Russia
3Clinical Resident, Department of Pediatric Surgery and Pediatrics, Institute of
Continuing Education, Kursk State Medical University, (Kursk, Russian Federation), Russia
*Address for Correspondence: Severinov DA, Associate Professor at the Department of Pediatric Surgery and Pediatrics, Institute of Continuing Education, Kursk State Medical University (Kursk, Russian Federation), Russia E-mail: [email protected]
Mesenteric cysts and cystic mesenteric tumors are very rare abdominal growths. They may be localized all over the mesentery, from the duodenum to the rectum, however, they are mostly found in the ileum and right colon mesentery. There are several classifications of these formations, among which the one based on histopathologic features including 6 groups has been most commonly used: 1) cysts of lymphatic origin--lymphatic (hilar cysts) and lymphangiomas; 2) cysts of mesothelial origin--benign or malignant mesothelial cysts; 3) enteric cysts; 4) cysts of urogenital origin; 5) dermoid cysts; and 6) pseudocysts-infectious or traumatic etiology.
A dermoid cyst is a benign, epithelial-lined cavitary lesion composed of ectoderm and mesoderm that can arise anywhere in the body, with a tendency to develop in midline structures.
In 20% - 45% of cases, accompanying diseases that were not previously clinically manifested can be diagnosed during emergency interventions, requiring additional surgical interventions for their correction.
The aim of the study is to demonstrate the successful treatment experience of a dermoid cyst of the mesentery of the jejunum, detected after traditional appendectomy.
Clinical case: A mother brought her 9-year-old son, V., to the emergency department of the Kursk Regional Children’s Clinical Hospital with complaints of moderate-intensity pain in the right iliac region, multiple episodes of vomiting, and fever. Ultrasound features indicative of destructive appendicitis and peritonitis. In an emergency situation, after preoperative preparation, a traditional appendectomy was performed under intravenous anesthesia, using the Volkovich-Dyakonov approach. The postoperative period was uneventful. Moderate infiltration was observed on the control abdominal ultrasound examination, in the intestine (presumably the small intestine) in the right half of the abdominal cavity, with a solid formation measuring 27*33 mm, producing a dense acoustic shadow. On the 7th day after the initial intervention, a revision of the abdominal organs was performed. The loop of the jejunum with the formation was brought out into the wound. The capsule above the formation was dissected: the formation of bone density, when the capsule is separated, resembles a fecal stone in structure, considering the localization - a dermoid cyst. Step-by-step enucleation of the cyst was performed. The postoperative wound was tightly sutured in layers.
One of the most common urgent pathologies in pediatric abdominal surgery is acute appendicitis. For many decades, acute appendicitis remains a disease associated with diagnostic and treatment complexity [1,2]. The wide range of clinical symptoms and the lack of pathognomonic signs present significant challenges in diagnosing specific abdominal pathologies [3].
Furthermore, it should be noted that in 20% - 45% of cases, accompanying diseases that were not previously clinically manifested can be diagnosed during emergency interventions, requiring additional surgical interventions for their correction [4,5].
Dermoid cysts can occur in different regions of the body. Abdominal dermoid cysts are very rare in the pediatric population. They can present in the acute setting by causing complications such as cyst rupture or intestinal volvulus. We are presenting a rare case of a dermoid cyst that presented with an acute abdomen.
The aim of the study is to demonstrate the successful treatment experience of a dermoid cyst of the mesentery of the jejunum, detected after traditional appendectomy.
A mother brought her 9-year-old son, V., to the emergency department of the Kursk Regional Children’s Clinical Hospital with complaints of moderate-intensity pain in the right iliac region, multiple episodes of vomiting, and fever. According to the mother, the boy has been sick for the past 24 hours, when he first experienced the above-mentioned symptoms. The abdominal pain has been worsening over time.
Upon admission, the overall condition of the patient was of moderate severity and stable. There was no vomiting or nausea. The patient was fully conscious. The body temperature was 36.8°C. The abdomen appeared normal in shape and not distended. Appendicular symptoms (Rovsing’s, Sitkovsky’s, Bartomie-Michelson’s) were positive. Peritoneal signs (Shchetkin-Blumberg’s, Voskresensky’s) were negative.
The following instrumental diagnostic methods were performed upon admission
Abdominal ultrasound: in the right iliac region, there was a vermiform appendix with a diameter of up to 17 mm, thickened walls, and a fluid component at the tip. In the right lateral canal and in the pelvis, there was heterogeneous fluid measuring up to 50 mm in height. Ultrasound features indicative of destructive appendicitis and peritonitis. In the complete blood count, there was leukocytosis, which indirectly indicates the presence of an inflammatory process in the abdominal cavity.
Given the above information, a preliminary diagnosis of Acute Appendicitis was made. In an emergency situation, after preoperative preparation, a traditional appendectomy was performed under intravenous anesthesia, using the Volkovich-Dyakonov approach. The appendix was retrocecal, located at the base, subserous, gray in color, rigid, approximately 10.0 cm in length, with a diameter of up to 0.9 cm along its length. From the base to the middle third, it was expanded to a diameter of 2 cm. A large fecal stone was palpated within the lumen. The appendix was gradually mobilized from adhesive adhesions. A typical appendectomy was performed with the invagination of the appendix stump into the dome of the cecum using purse-string and Z-shaped sutures. The wound was closed tightly in layers.
The postoperative period was uneventful. Moderate infiltration was observed on the control abdominal ultrasound examination, in the intestine (presumably the small intestine) in the right half of the abdominal cavity, with a solid formation measuring 27*33 mm, producing a dense acoustic shadow. A foreign body in the lumen of the small intestine (?) is suspected, a formation in the small intestine resembling a fecal stone of dense consistency (?), or a bezoar in the jejunum.
To confirm the diagnosis, a computed tomography scan of the abdominal organs and retroperitoneal space with intravenous contrast enhancement was performed. In the right side of the abdominal cavity at the level of L3-L4, an additional structure was visualized, resembling the shape of the number 8, measuring 32*20*36 mm, with a thick-walled capsule up to 3.5 mm thick and homogeneous content, with a volume of up to 8.5 ml. The obtained data may correspond to a foreign body in the right abdominal cavity.
A decision was made to perform a video laparoscopic revision of the abdominal organs with subsequent correction of the intraoperative tactics.
Under endotracheal anesthesia, on the 7th day after the initial intervention, a revision of the abdominal organs was performed. The peritoneum is smooth and shiny. The dome of the cecum is found, and the resection area of the appendix is intact. Further revision reveals a formation measuring 5*3.5*2 cm in the right half of the abdominal cavity, which is dense, fixed to a loop of small intestine, double-chambered, and mobile - it moves along with the loop of intestine. Upon detailed examination, the formation is found to originate from the mesentery of the jejunum, 1.8 m away from the ileocecal angle. It is covered with a capsule with a vascular component and is located along the mesenteric edge of the intestine. The loop of the jejunum is lowered to the appendectomy area.
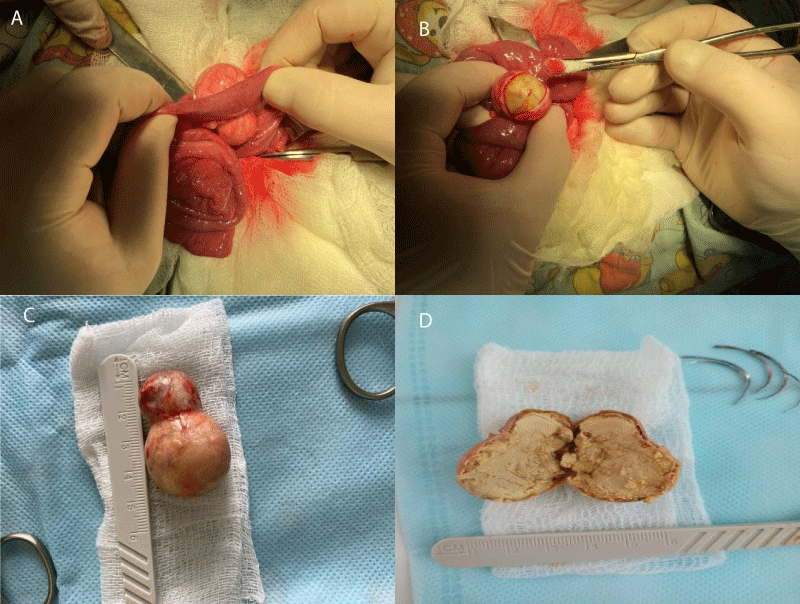
The sutures in the area of the postoperative wound in the right iliac region have been removed, and the tissues have been dissected in layers. The loop of the jejunum with the formation was brought out into the wound. The capsule above the formation was dissected: the formation of bone density, when the capsule is separated, resembles a fecal stone in structure, considering the localization - a dermoid cyst (Figure 1). Step-by-step enucleation of the cyst was performed. The postoperative wound was tightly sutured in layers. Aseptic dressing.
Figure 1: Intraoperative photo: laparotomy, A - surgeon's hands holding a loop of the jejunum with a formation; B - cyst capsule opened; C - view of the removed cyst; D - cyst incised longitudinally.
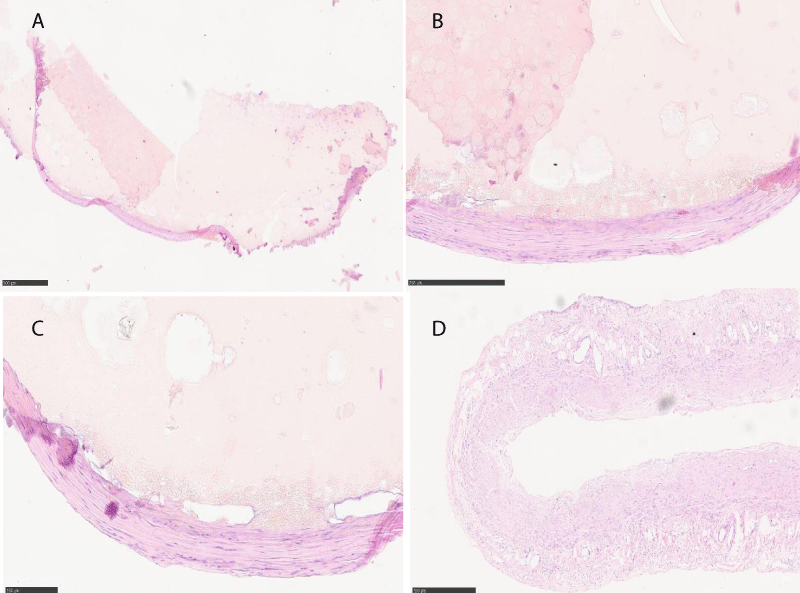
The histological examination (Figure 2) confirmed the histopathological structure of the dermoid cyst (fragments appear as grey-colored shells with thick walls, measuring up to 2.5/1 cm. Additionally, there is a significant amount of dried tissue in the form of shells with thin walls, overlaid on one of the surfaces with loose grayish-yellow masses. Furthermore, there is a separate large quantity of gray loose masses measuring 4/4 cm). The final clinical diagnosis was acute gangrenous appendicitis. Serous peritonitis. Dermoid cyst of the mesentery of the jejunum.
Figure 2: Histological photos, hemotaxylin and eosin coloration: A - 100-fold increase; B, C - 200-fold increase; D - 40-fold increase.
The boy was discharged in satisfactory condition on the 12th day since hospitalization.
Mesenteric cysts are a rare group of lesions that have been classified into six subtypes based on their histopathology.
These include
- Cysts of lymphatic origin (lymphangioma);
- Cysts of mesothelial origin (benign cystic mesothelioma, malignant cystic mesothelioma);
- Cysts of enteric origin (duplication cyst);
- Cysts of urogenital origin;
- Mature cystic teratoma (dermoid cysts), and
- Pseudocysts (infectious and traumatic cysts)
Dermoid cysts are commonly described in the head, neck, gonads, mediastinum, retroperitoneal and sacrococcygeal regions. There are four case reports in English literature of dermoid cysts occurring in the mesentery of children.
Dermoid cysts are postulated to occur as a result of abnormal migration of primordial germ cells. This is a complex and poorly understood process, reliant on a host of migratory and homing factors, making it difficult to explain why our patient’s cyst occurred at the mesentery of the jejunum region. We can only postulate that these cells may have migrated from the dorsal mesogastrium, in the midline, and then traversed in the mesentery of the jejunum region.
Patients with mesenteric dermoid cysts present in various ways. They may be identified incidentally. They can present as a slow-growing intraabdominal mass. They may cause vague gastrointestinal symptoms or present with acute pain due to cyst rupture or intestinal volvulus.
The described clinical observation demonstrates the complexity and multifaceted nature of approaches to the management of patients with acute appendicitis. There is a high likelihood of identifying concurrent surgical anomalies, both intraoperatively and during the stage of performing follow-up diagnostic investigations. This further contributes to the adjustment of the therapeutic approach and timely assistance to patients with rarely encountered surgical pathologies. The uniqueness of this case confirms the thesis that in the modern stage of development of applied medicine, a specialist, particularly a surgeon, should possess not only deep expertise in their field but also theoretical knowledge in related areas of medicine.
Authors’ contributions
All authors made equal contributions to the study and the publication.
All authors have read and approved the final version of the manuscript of the article. All authors agree to bear responsibility for all aspects of the study to ensure proper consideration and resolution of all possible issues related to the correctness and reliability of any part of the work.
Consent for publication
Written consent was obtained from the patients or their legal representatives for the publication of relevant medical information and all of the accompanying images within the manuscript.
- Svensson JF, Patkova B, Almström M, Eaton S, Wester T. Outcome after introduction of laparoscopic appendectomy in children: A cohort study. J Pediatr Surg. 2016 Mar;51(3):449-53. doi: 10.1016/j.jpedsurg.2015.10.002. Epub 2015 Nov 10. PMID: 26655215.
- Zhang S, Du T, Jiang X, Song C. Laparoscopic Appendectomy in Children With Perforated Appendicitis: A Meta-Analysis. Surg Laparosc Endosc Percutan Tech. 2017 Aug;27(4):262-266. doi: 10.1097/SLE.0000000000000411. PMID: 28472016.
- Zhang Z, Wang Y, Liu R, Zhao L, Liu H, Zhang J, Li G. Systematic review and meta-analysis of single-incision versus conventional laparoscopic appendectomy in children. J Pediatr Surg. 2015 Sep;50(9):1600-9. doi: 10.1016/j.jpedsurg.2015.05.018. Epub 2015 Jun 3. PMID: 26095165.
- Timerbulatov VM, Mekhdiev DI, Timerbulatov SV, Sagitov RB, Yamalov RA, Gaynullina EN. [Simultaneous abdominal and retroperitoneal surgery]. Khirurgiia (Mosk). 2016;(3):40-44. Russian. doi: 10.17116/hirurgia2016340-44. PMID: 27070874.
- Poddubny IV, Isaev AA, Ternavsky AP. Simulated laparoscopic operations in pediatric surgery. Surgeon. 2008; 12:48-57. (In Russ.).