More Information
Submitted: September 29, 2023 | Approved: October 09, 2023 | Published: October 10, 2023
How to cite this article: Askmyr D, Tjernström F. Case Report: Carotidynia Correlated to Cancer Treatment? Arch Case Rep. 2023; 7: 050-052.
DOI: 10.29328/journal.acr.1001078
Copyright License: © 2023 Askmyr D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Carotidynia; Neck pain; Chemotherapy; G-CSF
Case Report: Carotidynia Correlated to Cancer Treatment?
David Askmyr* and Fredrik Tjernström
and Fredrik Tjernström
Department of Otorhinolaryngology, Head and Neck Surgery, Skane University Hospital, Lund, Sweden
*Address for Correspondence: David Askmyr, Departtment of Otorhinolaryngology, Head and Neck Surgery, Skane University Hospital, 221 85, Lund, Sweden, Email: [email protected]
Carotidynia refers to an idiopathic, self-limiting, benign condition of head and neck pain emanating from a tender carotid artery. We report a case where a patient presenting with carotidynia combined with fever elevated white blood count and C-reactive protein (CRP), nine days after treatment with chemotherapy (paclitaxel-carboplatin) and granulocyte-colony stimulating factor (G-CSF). The condition resolved after treatment with glucocorticoids in combination with antibiotics. The radiological findings were congruent with caritodynia and the conclusion from the case was that the anti-cancer treatment was causative, supported by the literature reviewed, although paclitaxel has previously not been implicated.
Carotidynia was first described by Temple Fay in 1927 [1] though the condition didn’t gain status as a distinct disease entity until 1988 by the International Headache Society (IHS) [2]. The criteria proposed are listed in Table 1. With improved imaging technology in the 1990s, some of the cases previously defined as carotidynia turned out to be vascular diseases such as carotid dissection and arteritis [3,4]. Hence, when the IHS updated the classification in 2003, carotidynia was degraded to the appendix.
| Table 1: Criteria stated by the International Headache Society (IHS)) 1988. |
| A. At least one of the following overlying the carotid artery |
| 1. Tenderness |
| 2. Swelling |
| 3. Increased pulsations |
| B. Appropriate investigations not revealing structural abnormality |
| C. Pain over the affected side of the neck; may project to the ipsilateral side of the head |
| D. A self-limiting syndrome of less than 2 weeks’ duration |
Despite the lack of internationally accepted criteria, many authors today agree that carotidynia exists as a syndrome of pain in the head and neck, with distinct palpable tenderness over the carotid bifurcation (Fay’s sign). The pain is typically unilateral and is often aggravated by turning of head, swallowing, coughing, etc. As it is self-limiting within weeks in most reported cases, the proposed treatment varies from expectance to anti-inflammatory drugs such as NSAID or corticosteroids. The nomenclature has been debated, and carotiditis or carotid periarteritis has been suggested as a more accurate designation [5,6]. The possibility of designating the condition as a subset of vasculitis has also been advocated [7]. Specific structural radiographic findings associated with the symptoms of caritodynia have been described in the literature [8].
MRI findings include swelling of the soft tissue surrounding the carotid bifurcation, thickening of the vessel wall, and possibly a marginally decreased lumen though an affected circulation can be detected on neither MRI, CT nor ultrasound [9,10]. The outer layers of the artery are involved, but not the intima [11]. There are also histological case reports that verify a low-grade inflammation of the artery [12,13].
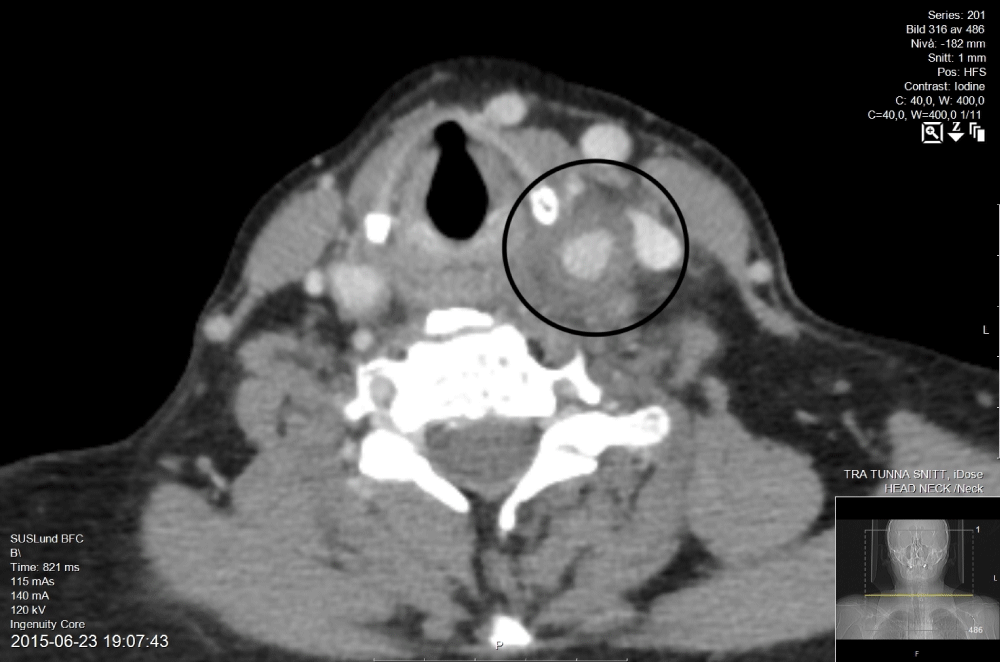
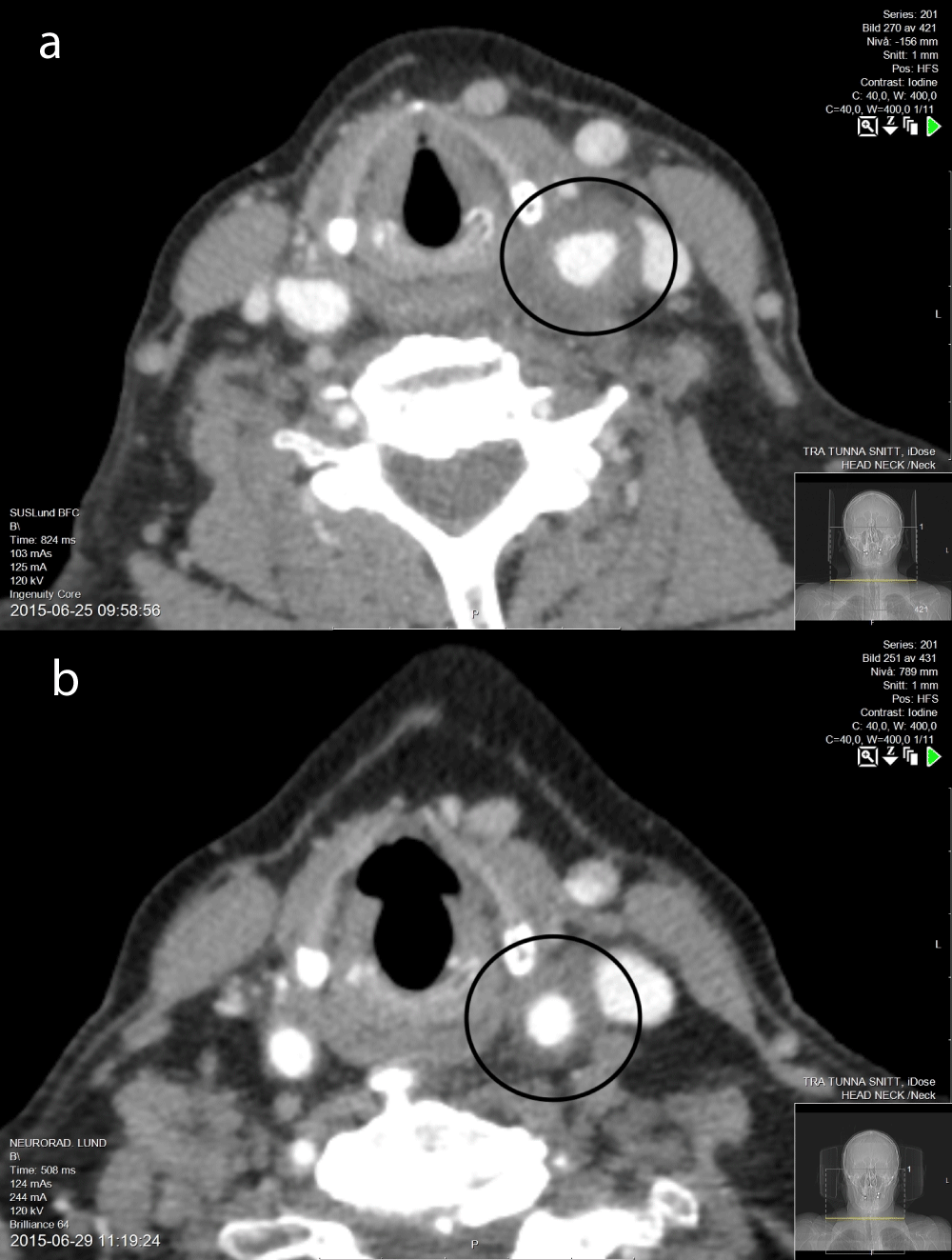
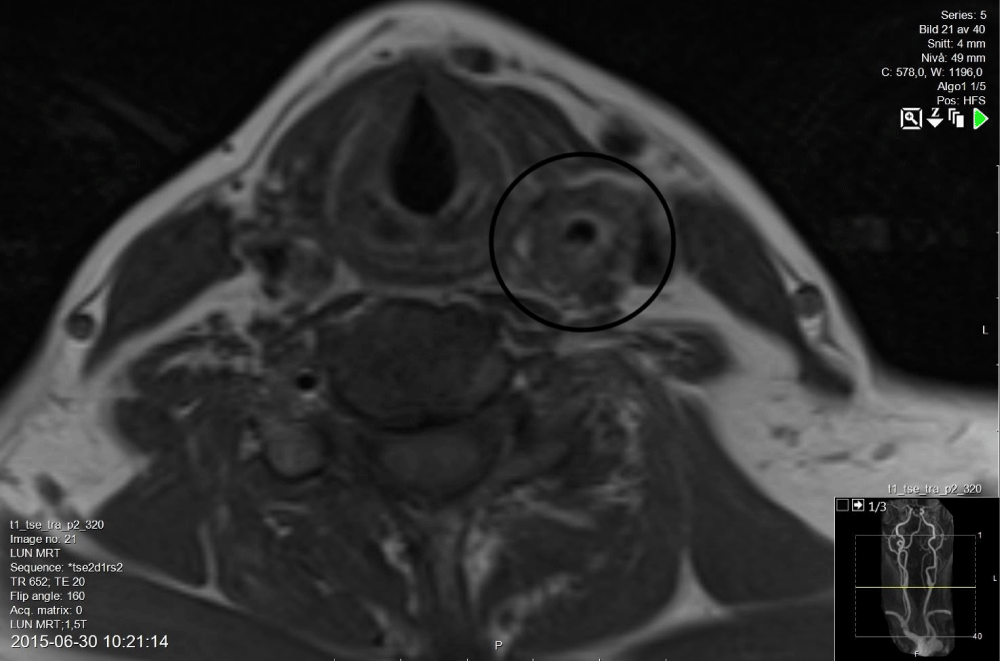
A 64-year-old woman suffering from generalized ovarian cancer was referred to the infectious disease department with a history of four days with intermittent fever and increasing pain in the left side of her face and neck. Nine days before the onset she had received her last treatment with chemotherapy (Paclitaxel-Carboplatin), and one day later she was treated with the Granulocyte-Colony Stimulating Factor (G-CSF) pegfilgrastim. On examination, she was extremely tender under her left mandibular angle and was found to have a poor dental status. CRP was 277 mg/L and body temperature 37,9 °C. Her blood count was de-arranged due to the G-CSF treatment with leukocytes 40000 whereof neutrophils 34000. A dental infection was suspected and she was referred to the ENT clinic. Further examination revealed a pronounced soreness over her left carotid artery. The patient received antibiotic i.v. (Piperacillin/Tazobactam 4g x 3) and underwent an acute CT scan, that confirmed a diffuse swelling of the soft tissue surrounding the common carotid artery and more cranial the internal and external carotid artery. No signs of abscess were seen, and the radiology report suggested metastasis as a possible explanation (Figure 1). Due to the clinical presentation, caritodynia was immediately suspected, and supported by a PUBMED search where taxanes and G-CSF have been implicated as causative in carotidynia. Treatment with antibiotics continued since the blood tests were elevated in combination with fever. Differential diagnoses such as metastasis or other forms of vasculitis were discussed and discarded. On the 2nd day corticosteroid treatment was initiated (40 mg Prednisolone daily) and continued until recovery. During the following days, the patient underwent two additional CT scans that indicated regression of the swelling around the artery (Figure 2). After seven days the neck pain was gone, CRP was reduced to 50 mg/L and the patient subjectively recovered. She was discharged with Prednisolone in tapering dosage together with Clindamycin. No culture was positive (blood, naso- and oropharynx). On the day of discharge, an MRI still showed a thickened carotid wall involving the tunica adventitia and media, with the intima and lumen intact (Figure 3). The patients’ oncologist considered the cancer treatment as the most possible cause of the carotidynia, and future treatment excluded both Paclitaxel and G-CSF. CRP was normalized 20 days after the onset of symptoms, and during a follow-up period of six months, the pain did not recur.
Figure 1: CT scan day 1 shows accumulation of contrast in the tissue surrounding the carotid sheet.
Figure 2: CT scans day 3 (a) shows an unchanged swelling of the tissue surrounding the carotid sheet, while in day 7 (b) it has partially decreased, with a remaining swelling within the carotid sheet.
Figure 3: The MRI on day 8 present a thickened carotid wall involving the tunica adventitia and media, with the intima and lumen intact.
The patient in the reported case presented with symptoms and radiological findings congruent with carotidynia. The onset of pain was nine days after treatment with paclitaxel and eight days after G-CSF administration, which induced us to suspect either of those as a triggering factor. This theory is to some extent supported by other case reports. To our knowledge carotidynia after paclitaxel treatment never has been reported before, but the use of another taxane (docetaxel) as well as G-CSF has previously been implicated as causative agents of carotidynia [14-17]. Similar to our case the onset was usually delayed after treatment and also combined with fever and increased inflammatory parameters in blood tests. These parameters are not typically enhanced in carotidynia but rather suggest a more severe form of the condition when occurring simultaneously with anti-cancer treatment. The clinical challenge is thus to recognize the condition, refrain from surgery (on the suspicion of abscess), and instead start potent anti-inflammatory treatment.
G-CSF has a range of pro-inflammatory effects and is known to be a causative agent of cutaneous vasculitis [18] as well as exacerbating other forms of vasculitis [19]. Two cases of aortitis after G-CSF treatment have also been reported, of which one also had received docetaxel [20,21].
The reported case indicates that anti-cancer treatment may be capable of triggering carotidynia. The authors have no conclusion as to whether the chemotherapy or the G-CSF is more likely to be the causative agent, nor what mechanisms may be involved. There is also a chance that the relationship between treatment and illness is only temporally and that further treatment might not induce the condition again. Future studies and reports hopefully will address these issues. The case also highlights the use of imaging in distinguishing acrodynia from other causes of neck pain and signs of inflammation.
Ethical considerations: The patient agreed to participate in the case report.
- Fay T. Atypical neuralgia. Arch neurol psychiatry. 1927; 18:309-315.
- Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia. 1988;8 Suppl 7:1-96. PMID: 3048700.
- Biousse V, Bousser MG. The myth of carotidynia. Neurology. 1994 Jun;44(6):993-5. doi: 10.1212/wnl.44.6.993. PMID: 8208434.
- Biousse V, Woimant F, Amarenco P, Touboul PJ, Bousser MG. Pain as the only manifestation of internal carotid artery dissection. Cephalalgia. 1992 Oct;12(5):314-7. doi: 10.1046/j.1468-2982.1992.1205314.x. PMID: 1423563.
- Hafner F, Hackl G, Haas E, Eller P, Gstettner C, Vollmann R, Brodmann M. Idiopathic carotidynia. Vasa. 2014 Jul;43(4):287-92. doi: 10.1024/0301-1526/a000365. PMID: 25007908.
- Tardy J, Pariente J, Nasr N, Peiffer S, Dumas H, Cognard C, Larrue V, Chollet F, Albucher JF. Carotidynia: a new case for an old controversy. Eur J Neurol. 2007 Jun;14(6):704-5. doi: 10.1111/j.1468-1331.2007.01776.x. PMID: 17539956.
- Taniguchi Y, Horino T, Hashimoto K. Is carotidynia syndrome a subset of vasculitis? J Rheumatol. 2008 Sep;35(9):1901-2. PMID: 18785305.
- Syms MJ, Burton BS, Burgess LP. Magnetic resonance imaging in carotidynia. Otolaryngol Head Neck Surg. 1997 Dec;117(6):S156-9. doi: 10.1016/S0194-59989770088-3. PMID: 9419134.
- Buetow MP, Delano MC. Carotidynia. AJR Am J Roentgenol. 2001 Oct;177(4):947. doi: 10.2214/ajr.177.4.1770947. PMID: 11566713.
- Schaumberg J, Eckert B, Michels P. Carotidynia: magnetic resonance imaging and ultrasonographic imaging of a self-limiting disease. Clin Neuroradiol. 2011 Jun;21(2):91-4. doi: 10.1007/s00062-010-0042-5. Epub 2011 Jan 19. PMID: 21246181.
- Stanbro M, Gray BH, Kellicut DC. Carotidynia: revisiting an unfamiliar entity. Ann Vasc Surg. 2011 Nov;25(8):1144-53. doi: 10.1016/j.avsg.2011.06.006. PMID: 22023945.
- Farage L, Motta AC, Goldenberg D, Aygun N, Yousem DM. Idiopathic inflammatory pseudotumor of the carotid sheath. Arq Neuropsiquiatr. 2007 Dec;65(4B):1241-4. doi: 10.1590/s0004-282x2007000700030. PMID: 18345439.
- Upton PD, Smith JG, Charnock DR. Histologic confirmation of carotidynia. Otolaryngol Head Neck Surg. 2003 Oct;129(4):443-4. doi: 10.1016/S0194-59980300611-9. PMID: 14574303.
- Azar L, Fischer HD. Perivascular carotid inflammation: an unusual case of carotidynia. Rheumatol Int. 2012 Feb;32(2):457-9. doi: 10.1007/s00296-009-1309-5. Epub 2009 Dec 20. PMID: 20091034.
- Bendix N, Glodny B, Bernathova M, Bodner G. Sonography and CT of vasculitis during gemcitabine therapy. AJR Am J Roentgenol. 2005 Mar;184(3 Suppl):S14-5. doi: 10.2214/ajr.184.3_supplement.01840s14. PMID: 15728007.
- Cassone G, Colaci M, Giuggioli D, Manfredi A, Sebastiani M, Ferri C. Carotidynia Possibly due to Localized Vasculitis in a Patient with Latent Mycobacterium tuberculosis Infection. Case Rep Vasc Med. 2013;2013:585789. doi: 10.1155/2013/585789. Epub 2013 Dec 2. PMID: 24363952; PMCID: PMC3864074.
- Hayashi S, Maruoka S, Takahashi N, Hashimoto S. Carotidynia after anticancer chemotherapy. Singapore Med J. 2014 Sep;55(9):e142-4. doi: 10.11622/smedj.2014127. PMID: 25273942; PMCID: PMC4293954.
- Jain KK. Cutaneous vasculitis associated with granulocyte colony-stimulating factor. J Am Acad Dermatol. 1994 Aug;31(2 Pt 1):213-5. doi: 10.1016/s0190-9622(94)70149-0. PMID: 7518847.
- Freeley SJ, Coughlan AM, Popat RJ, Dunn-Walters DK, Robson MG. Granulocyte colony stimulating factor exacerbates antineutrophil cytoplasmic antibody vasculitis. Ann Rheum Dis. 2013 Jun;72(6):1053-8. doi: 10.1136/annrheumdis-2012-202160. Epub 2012 Oct 19. Erratum in: Ann Rheum Dis. 2022 Oct;81(10):e212. PMID: 23087180.
- Adiga GU, Elkadi D, Malik SK, Fitzpatrick JD, Madajewicz S. Abdominal aortitis after use of granulocyte colony-stimulating factor. Clin Drug Investig. 2009;29(12):821-5. doi: 10.2165/11530790-000000000-00000. PMID: 19888788.
- Darie C, Boutalba S, Fichter P, Huret JF, Jaillot P, Deplus F, Gerenton S, Zenone T, Moreau JL, Grand A. Aortite après injections de G-CSF [Aortitis after G-CSF injections]. Rev Med Interne. 2004 Mar;25(3):225-9. French. doi: 10.1016/j.revmed.2003.10.015. PMID: 14990294.