More Information
Submitted: August 11, 2023 | Approved: September 05, 2023 | Published: September 06, 2023
How to cite this article: Peña BR, Vazquez VP, de Lara Banhadan V, Luque CJ, Guerrero JLA, et al. Deep Venous Thrombosis as the Clinical Expression of POEMS Syndrome. Arch Case Rep. 2023; 7: 038-041.
DOI: 10.29328/journal.acr.1001075
Copyright License: © 2023 Peña BR, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abbreviations: TSH: Thyroid-Stimulating Hormone; ANA: Antinuclear Antibody; VEGF: Vascular Endothelial Growth Factor; CT: Computed Tomography; EMG: Electromyography
Deep Venous Thrombosis as the Clinical Expression of POEMS Syndrome
Beatriz Rosado Peña1, Virginia Perez Vazquez2, Victoria de Lara Banhadan3, Carlos Jarava Luque2, Jose Luis Andrey Guerrero2 and Juan-Bosco Lopez-Saez2*
1Neurophisiology Department, The University of Cadiz, Cadiz, Spain
2Internal Medicine Department, The University of Cadiz, Cadiz, Spain
3Radiologist Department, University Hospital of Puerto Real, The University of
Cadiz, Cadiz, Spain
*Address for Correspondence: Juan-Bosco Lopez-Saez, MD, Ph.D., Department of Internal Medicine, The University of Cadiz, c/. Dr. Marañon, 6, 11003-Cadiz, Spain, Email: [email protected]
This case suggests that POEMS syndrome does present with a constellation of signs and symptoms that may lead a clinician to a multitude of other possible diagnoses. Diagnosis is often difficult and delayed. A good history and physical examination as well as a careful review of all workups are paramount in establishing this particular diagnosis. The major criteria of diagnostic for the syndrome are polyradiculoneuropathy, clonal plasma disorder, sclerotic bone lesions, the presence of Castleman disease, and elevated vascular endothelial growth factor. Minor features include organomegaly, extravascular volume overload, endocrinopathy, characteristic skin changes, papilledema, and thrombocytosis. The diagnosis is made with three of the major criteria, two of which must include polyradiculoneuropathy and clonal plasma cell disorder, and at least one of the minor criteria. In this article, we discuss the differential diagnosis and outline the clinical evaluation indicated.
We present a case of POEMS syndrome that started who presented a deep vein thrombosis, as the first manifestation [1-4].
A 60-year-old female was admitted to our Hospital because the guiding symptom was swelling of the right leg. She had a positive Homans sign and was diagnosed with deep vein thrombosis. With a history of 6 years of disabling peripheral neuropathy treated with corticosteroids without improvement, followed by a progressive loss of strength in both lower limbs and general fatigue in November 2015. She also developed hypothyroidism and diabetes mellitus type 2, 1 year ago. The patient reported no history of exposure to toxins or a family history of neuropathy. She did not have Raynaud´s phenomenon. On physical examination revealed hypertrichosis on his forearms and mild edema of the lower limbs, hepatosplenomegaly, and lymphadenopathy. Three months later, we noted that she presented with general cutaneous pigmentation and sclerotic skin changes in her forearms and hands. She exhibited dry skin on her extremities, and general edema, especially of the lower limbs. He had modest skin sclerosis on his fingers and the dorsum of the hands as well as a contracture of the finger joints. She had lost approximately 12 kg over the course of a year and suffered from diarrhea. Neurological examination revealed moderate muscle weakness and mild sensory disturbance in both lower limbs. The Achilles tendon reflex was absent bilaterally, and the other deep tendon reflexes were hyporesponsive. The cranial nerves were normal. Her home medications included levothyroxine 75 pg once daily, metformin 850 mg bid, and enoxaparin 100 mg once daily [5-8].
Laboratory data
Complete blood count showed a white blood count of 8.800 mm3, hemoglobin of 10.4 g/dL, hematocrit of 31.9%, platelets of 306.000 per mm3, and D-dimer 23.6 pg/dL. Also, laboratory testing showed slightly elevated levels of blood urea nitrogen (44 mg⁄dL), renal dysfunction (serum creatinine 1.81 g/dL), C-reactive protein (4.5 mg⁄dL), erythrocyte sedimentation rate (70 mm⁄h) and hemoglobin A1c was 7.8%. The levels of TSH and anti-thyroid antibodies were high as well: (TSH: 6.3 IU/ml; anti microsomal 28.3 IU/mL, antiTPO: 6.7 IU/mL). Although serum levels of immunoglobulin IgG (1690 mg⁄dL) and IgM (142 mg⁄dL) were within normal range, serum IgA levels (573 mg⁄dL) were elevated and all protein was detected by immunoelectrophoresis of serum. Bence–Jones protein was negative in urine. The results of ANA testing were positive at 1:320, but test results for other autoimmune and peripheral neuropathy autoantibodies were negative. In this patient, HIV, vitamin B12, and test results were normal. Plasma VEGF levels were markedly elevated (634 pg⁄mL) [9-12].
Echocardiography data
Transthoracic echocardiography revealed normal left ventricular volumes and ejection fraction, mild pericardial effusion, severe tricuspid regurgitation, and pulmonary hypertension (systolic pulmonary artery pressure was 80 mmHg). Neither intracardiac thrombus nor evidence of akinetic or hypokinetic segments, which may contribute to cardiac emboli, was detected on transthoracic echocardiography.
Radiologic data
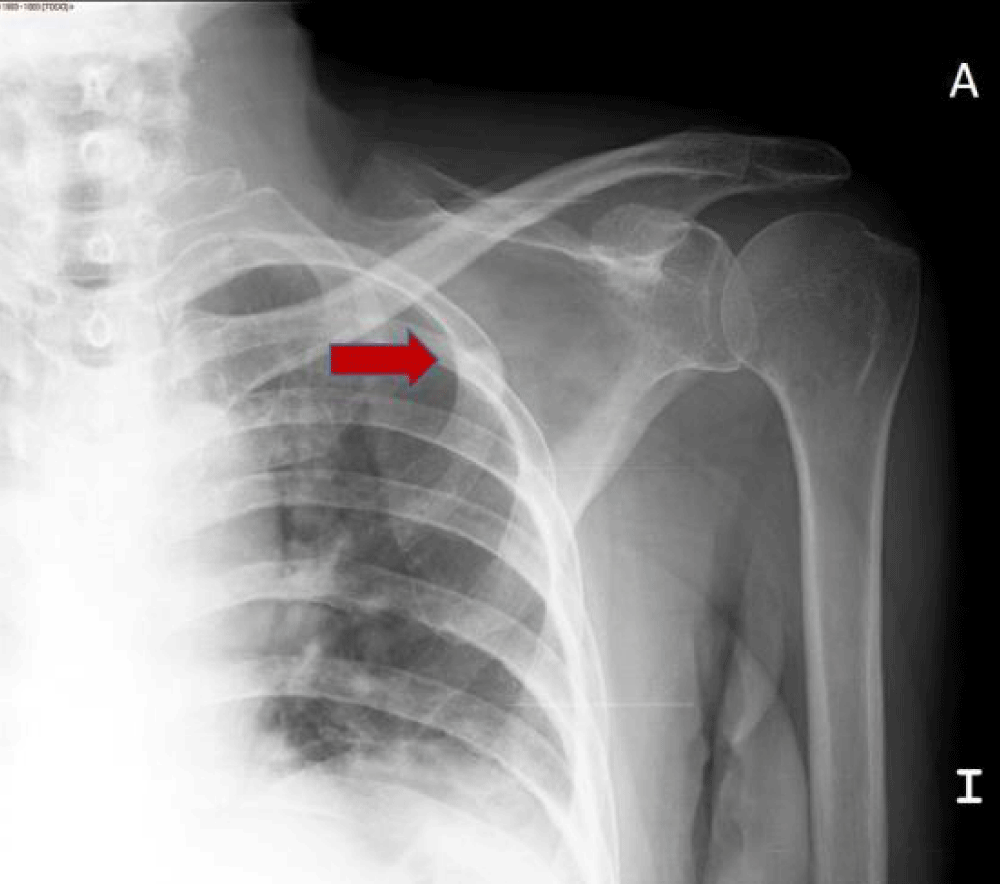
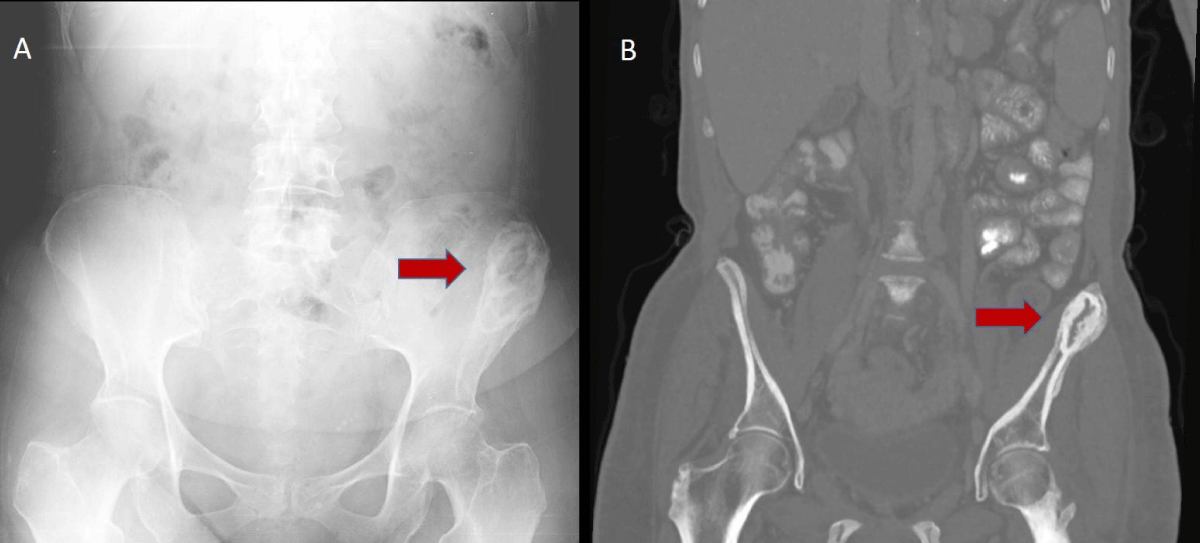
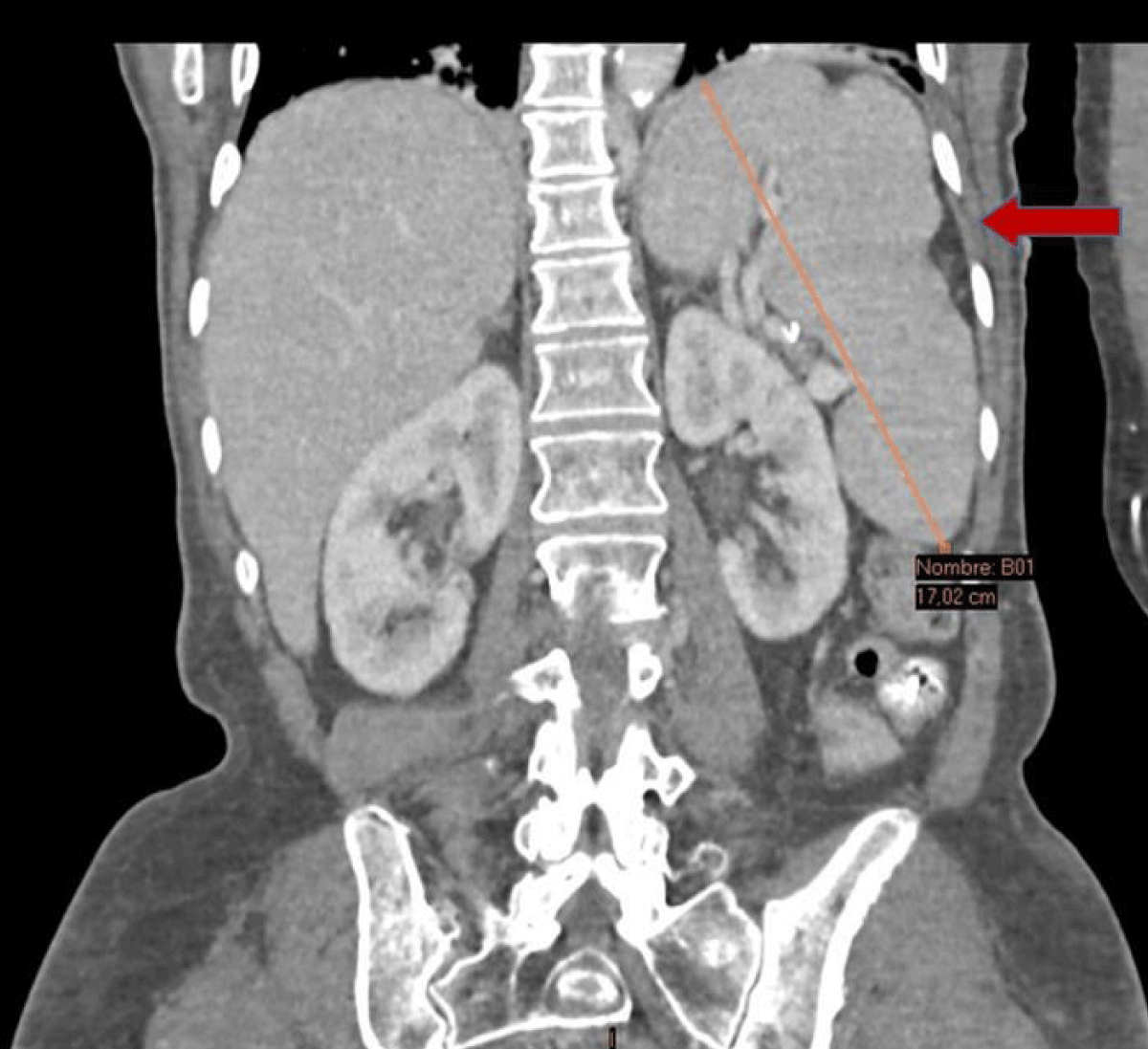
The Doppler ultrasound study of both legs showed a thrombosis from the iliac, femoral, and left popliteal veins. CT of the chest showed pericardial effusion and bilateral pleural effusions. Skeletal radiology and CT examination revealed osteosclerotic lesions but not osteolytic lesions. The findings are consistent with previous reports of bone lesions in patients with POEMS syndrome. With the diagnosis of POEMS syndrome, a serial bone study was performed, which showed focal sclerous lesions in the second left costal arch (Figure 1). An abdominal CT was also performed to better identify the pelvic bone lesion. The left iliac blade lesion had a mixed component with a central radiolucent zone surrounded by a sclerous annular margin, different from the pure lytic aspect of classic myeloma (Figure 2). In our patient’s pelvic tomography, an expansive lesion was reported at the level of the posteromedial border of the left iliac with periosteal reaction, bone matrix, and thickening towards the adjacent soft tissues (Figure 2). An abdominal CT showed moderate hepatomegaly and splenomegaly (Figure 3) [13-16].
Figure 1: A proximal humerus radiograph showed well-defined sclerotic lesion in the second left rib.
Figure 2: a). A pelvic radiograph showed a large mixed sclerotic and lytic lesion in the left iliac bone. This lesion had sclerotic margins giving the typical ring-like appearance. b). The same injury but in CT scan study.
Figure 3: Contrast-enhanced CT scan showed organomegaly: enlarged spleen and moderate hepatomegaly.
Electromyography data
EMG reportedly showed prolonged F responses in both feet, normal motor and sensory responses in the distal segments of the arms, and no motor responses in the intrinsic foot muscles. A diagnosis of chronic inflammatory demyelinating polyneuropathy was made. A nerve conduction study could not detect sensory and motor nerve conduction velocity in the right tibial and peroneal nerves.
Histologic data
In the biopsy of the sclerotic skin lesions, demonstrated infiltration of plasma cells was observed, and also thickening of the collagen fibers in the middle and lower dermal layers, which is indicative of this syndrome. Histology of the bone marrow did not reveal an increase in the number of plasma cells.
We report here a case study describing a 60-year-old female with clinical features typical of POEMS syndrome. In this unique syndrome abnormalities occur in the central and peripheral nervous systems, the tegument, the endocrine glands, the skeleton, and the reticulo-entothelial and immunohematopoietic systems. The pathophysiological interrelationships among these systems are obviously complex and not well understood. Peripheral neuropathy is the dominant clinical feature of this disorder The diagnosis of POEMS syndrome was made based on the presence of polyneuropathy, mild hepatosplenomegaly, endocrinopathy, monoclonal gammopathy, and hypertrichosis. Two major criteria: polyneuropathy and monoclonal plasma proliferative disorder and at least 1 minor criterion: osteosclerotic myeloma, Castleman´s disease, organomegaly, endocrinopathy, edema, typical skin changes, and papilledema are required for diagnosis of POEMS syndrome defined by a retrospective review at Mayo Clinic. Since there is no single test that establishes the diagnosis, different signs and symptoms that must be put together to be able to diagnose polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes (POEMS) syndrome. The diagnosis is made based on a composite of clinical and laboratory features. Most notably, the constellation of peripheral neuropathy (especially demyelinating) and any of the following should elicit an in-depth search for POEMS syndrome: monoclonal protein (especially when restricted), thrombocytosis, anasarca, or papilledema. Serum levels of VEGF were markedly elevated during the active period of POEMS syndrome and subsequently decreased in response to therapy. However, it is well known that VEGF is a critical factor for neovascularization and acceleration of vasopermeability via targeting of endothelial cells. Increased VEGF could account for organomegaly, edema, skin hemangioma, and the occasional mesangioproliferative changes found on renal biopsy. We think that the elevation of VEGF may be the pathogenesis of thromboembolic disease.
Radiological bone lesions can be detected in 54% - 95% of the cases of POEMS syndrome. The characteristic appearance is that of one or several pure or mixed osteosclerotic focal lesions with a central radiolucent component surrounded by an annular sclerotic margin, with or without internal septa. The lesions predominate in the axial and proximal appendicular skeleton and may appear many years before diagnosis. The skull is usually respected. In flat bones, such as the pelvis and ribs, the lesions are often expansive, with periosteal reaction.
Clinical course
Weeks after her initial diagnostic evaluation, the patient was noted to have bilateral lower extremity edema and endorsed a few months of progressive skin hyperpigmentation on her face and distal extremities. Splenomegaly was identified on physical examination, measuring 18.5 cm on CT of the chest, abdomen, and pelvis. The patient was initially treated with prednisone, but her weakness worsened one month after the initiation of treatment, and after two months she was nearly bedridden. Due to the worsening, it was decided to start chemotherapy with melphalan (15 mg) orally, on days 1-14, and dexamethasone (40 mg) orally, on days 1–4 for 6 weeks. After five cycles of chemotherapy, skin thickening, and edema of lower and peripheral neuropathy began to slowly improve. Three years after the diagnosis, the patient began to temperate , going to the outpatient Internal Medicine, until she suffered a pulmonary infection, which required hospital admission the patient was worsened with a diagnosis of sepsis of respiratory origin until she died.
The POEMS syndrome is a multisystemic disease that is difficult to diagnose due to its low incidence and prevalence, together with the fact that the appearance of signs and symptoms does not occur simultaneously. Our patient suffered from 6 years of chronic peripheral neuropathy, and she had an extensive workup by multiple physicians. The natural course of the disease is chronic and the morbidity depends on the systems involved and the extent of the disease. In conclusion, POEMS syndrome should be considered in the differential diagnosis of patients presenting with a combination of peripheral neuropathy and thromboembolic events, particularly when a monoclonal protein in the serum is present.
- Dispenzieri A. POEMS syndrome: 2017 Update on diagnosis, risk stratification, and management. Am J Hematol. 2017 Aug;92(8):814-829. doi: 10.1002/ajh.24802. PMID: 28699668.
- Ohwada C, Sakaida E, Kawajiri-Manako C, Nagao Y, Oshima-Hasegawa N, Togasaki E, Muto T, Tsukamoto S, Mitsukawa S, Takeda Y, Mimura N, Takeuchi M, Shimizu N, Misawa S, Iseki T, Kuwabara S, Nakaseko C. Long-term evaluation of physical improvement and survival of autologous stem cell transplantation in POEMS syndrome. Blood. 2018 May 10;131(19):2173-2176. doi: 10.1182/blood-2017-07-795385. Epub 2018 Mar 29. PMID: 29599110; PMCID: PMC5946762.
- Karam C, Klein CJ, Dispenzieri A, Dyck PJ, Mandrekar J, D'Souza A, Mauermann ML. Polyneuropathy improvement following autologous stem cell transplantation for POEMS syndrome. Neurology. 2015 May 12;84(19):1981-7. doi: 10.1212/WNL.0000000000001565. Epub 2015 Apr 15. PMID: 25878176; PMCID: PMC4433461.
- Li Y, Valent J, Soltanzadeh P, Thakore N, Katirji B. Diagnostic challenges in POEMS syndrome presenting with polyneuropathy: A case series. J Neurol Sci. 2017 Jul 15;378:170-174. doi: 10.1016/j.jns.2017.05.019. Epub 2017 May 11. PMID: 28566158.
- Shibuya K, Misawa S, Horikoshi T, Kanai K, Isose S, Nasu S, Sekiguchi Y, Noto Y, Fujimaki Y, Nakaseko C, Kuwabara S. Detection of bone lesions by CT in POEMS syndrome. Intern Med. 2011;50(13):1393-6. doi: 10.2169/internalmedicine.50.5263. Epub 2011 Jul 1. PMID: 21720058.
- Li J, Zhou DB, Huang Z, Jiao L, Duan MH, Zhang W, Zhao YQ, Shen T. Clinical characteristics and long-term outcome of patients with POEMS syndrome in China. Ann Hematol. 2011 Jul;90(7):819-26. doi: 10.1007/s00277-010-1149-0. Epub 2011 Jan 8. PMID: 21221584.
- Gandhi GY, Basu R, Dispenzieri A, Basu A, Montori VM, Brennan MD. Endocrinopathy in POEMS syndrome: the Mayo Clinic experience. Mayo Clin Proc. 2007 Jul;82(7):836-42. doi: 10.4065/82.7.836. PMID: 17605964.
- Allam JS, Kennedy CC, Aksamit TR, Dispenzieri A. Pulmonary manifestations in patients with POEMS syndrome: a retrospective review of 137 patients. Chest. 2008 Apr;133(4):969-74. doi: 10.1378/chest.07-1800. Epub 2008 Jan 15. PMID: 18198255.
- Néel A, Hello M, Barbarot S, Jossic F, Masseau A, Espitia O, Mussini JM, Moreau P, Musset L, Hamidou M. Skin patch, polyneuropathy, and paraproteinemia. Am J Med. 2012 Dec;125(12):e1-2. doi: 10.1016/j.amjmed.2012.03.004. Epub 2012 Jul 25. PMID: 22840915.
- Mauermann ML, Sorenson EJ, Dispenzieri A, Mandrekar J, Suarez GA, Dyck PJ, Dyck PJ. Uniform demyelination and more severe axonal loss distinguish POEMS syndrome from CIDP. J Neurol Neurosurg Psychiatry. 2012 May;83(5):480-6. doi: 10.1136/jnnp-2011-301472. Epub 2012 Mar 6. PMID: 22396441.
- Dispenzieri A. How I treat POEMS syndrome. Blood. 2012 Jun 14;119(24):5650-8. doi: 10.1182/blood-2012-03-378992. Epub 2012 Apr 30. PMID: 22547581; PMCID: PMC3425020.
- Li J, Zhang W, Jiao L, Duan MH, Guan HZ, Zhu WG, Tian Z, Zhou DB. Combination of melphalan and dexamethasone for patients with newly diagnosed POEMS syndrome. Blood. 2011 Jun 16;117(24):6445-9. doi: 10.1182/blood-2010-12-328112. Epub 2011 Mar 10. PMID: 21393478; PMCID: PMC3123016.
- Misawa S, Sato Y, Katayama K, Hanaoka H, Sawai S, Beppu M, Nomura F, Shibuya K, Sekiguchi Y, Iwai Y, Watanabe K, Amino H, Ohwada C, Takeuchi M, Sakaida E, Nakaseko C, Kuwabara S. Vascular endothelial growth factor as a predictive marker for POEMS syndrome treatment response: retrospective cohort study. BMJ Open. 2015 Nov 11;5(11):e009157. doi: 10.1136/bmjopen-2015-009157. PMID: 26560063; PMCID: PMC4654348.
- Min JH, Hong YH, Lee KW. Electrophysiological features of patients with POEMS syndrome. Clin Neurophysiol. 2005 Apr;116(4):965-8. doi: 10.1016/j.clinph.2004.11.011. Epub 2004 Dec 15. PMID: 15792906.
- Brown R, Ginsberg L. POEMS syndrome: clinical update. J Neurol. 2019 Jan;266(1):268-277. doi: 10.1007/s00415-018-9110-6. Epub 2018 Nov 29. PMID: 30498913; PMCID: PMC6342878.
- Barete S, Mouawad R, Choquet S, Viala K, Leblond V, Musset L, Amoura Z, Khayat D, Francès C. Skin manifestations and vascular endothelial growth factor levels in POEMS syndrome: impact of autologous hematopoietic stem cell transplantation. Arch Dermatol. 2010 Jun;146(6):615-23. doi: 10.1001/archdermatol.2010.100. PMID: 20566924.