More Information
Submitted: November 29, 2019 | Approved: May 05, 2023 | Published: May 08, 2023
How to cite this article: Odionnys RL, Miriangel E, Yalisca P. Refractory priapism associated with anti-psychotics. Report of a case for risperidone. Arch Case Rep. 2023; 7: 020-022.
DOI: 10.29328/journal.acr.1001070
Copyright License: © 2023 Odionnys RL, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Priapism; Antipsychotics; Risperidone
Refractory priapism associated with anti-psychotics. Report of a case for risperidone
Ramos Luces Odionnys1*, Fermín Miriangel1 and Perdomo Yalisca2
1Specialist Physician of the General Adult Urology service, Hospital Miguel Pérez
Carreño, Caracas, Venezuela
2Postgraduate Residents of the Soft Surgery Service, Dr. José Ignacio Baldo
Hospital, Caracas, Venezuela
*Address for Correspondence: Ramos Luces Odionnys, Specialist Physician of the General Adult Urology service, Hospital Miguel Pérez Carreño, Caracas, Venezuela, Email: [email protected]
Priapism is a prolonged erection, usually painful, that occurs in the absence of sexual desire or stimulation, is not relieved by masturbation or intercourse and is the consequence of a mismatch in the regulatory mechanisms that initiate penile erection and those that allow its detumescence. One of the main causes of low-flow priapism is the use of drugs with an α-adrenergic antagonist effect, among which antipsychotic drugs stand out. Our objective is to present a clinical case and review the literature on the use of antipsychotics in medicine, psychiatry and other specialties and their relationship with the dose of the psychoactive drug in the onset of priapism. We present a 23-year-old male patient, single, with a significant history of mild Autism, for which he has received regular treatment with 6 mg daily of risperidone. He started experiencing priapism spontaneously for the last 4 days until a family member took him to the Emergency Room – intense, persistent and painful penile erection. Given the failure of the initial medical treatment for priapism, it was decided to perform multiple distal cavernous-cancellous shunts with improvement after 72 hours and discharge of the patient. We understand that there is a high affinity of antipsychotics for the α 1-adrenergic receptor, risperidone has an α 1 antagonist capacity. In fact, the third cause of priapism cases induced by atypical antipsychotics is secondary to risperidone, including recent cases associated with its parenteral depot presentation RisperdalConsta®.
Priapism is a term derived from Greek Priapus, representing the Greek and Roman God whose figure was related to seduction, fertility and sexual love, to which he was attributed therapeutic powers over male genital diseases in general. This god was also known for his giant phallus. The first recorded publication dates from 1616. Callaway in 1824 described the first case of priapism; since then attention has been limited to the study of incidence, etiology, physiopathology, diagnosis and timely treatment of Priapism. Priapism is associated with devastating psychosocial consequences and results unfavorable to the patient’s expectations that they can include irreversible and permanent erectile dysfunction [1,2].
The existence of epidemiologically well-designed, and community-based studies is limited. Recent data reveal that the incidence of priapism in the general population is low. A Finnish retrospective study determined that the incidence of priapism in the early years of the study ranged from 0.3 to 0.5 cases per 100,000 inhabitants/year. At the end of the study, they observed an increase in incidence to 1.1 cases per 100,000 inhabitants/year. The above was attributed to the new use of intracavernous vasoactive agents, introduced for the treatment of erectile dysfunction. Recently, Eland, et al. conducted a retrospective study taking the Integrated Primary Care database, which contains data from all patients that have been evaluated by general practitioners in the Netherlands. This study showed a slight increase in the incidence of non-iatrogenic priapism (0.9 cases per 100,000 inhabitants/year). The incidence of priapism in the United States and other countries where hemoglobinopathies such as falciform cell anemia are prevalent may be higher than in countries that do not present them. A study was conducted at five centers in the UK and Nigeria in which 130 patients were diagnosed with falciform cell anemia a 35% prevalence of priapism [3,4].
The Consensus for the Evaluation and Treatment of Priapism, under the auspices of the American Foundation for Urological Disease and with the multidisciplinary participation of experts in the area of pediatrics, hemato-oncology, psychiatry, and urology, defined priapism as “the pathological condition characterized by a penis erection that persists beyond or is not related to sexual stimulation.” Consensus also classified priapism in:
Ischemic priapism (veno-occlusive)
It is the most common form of priapism; it is usually presented with a painful erection and maximum rigidity, clinically characterized by the absence of cavernous blood flow. Ischemic priapism lasting more than 4 hours behaves as a compartmental syndrome and requires urgent medical intervention. The potential consequences are irreversible body fibrosis and permanent erectile dysfunction.
Arterial priapism (non-ischemic)
It is a less frequent appearance, caused by the entry of uncontrolled cavernous blood flow. The erection is generally not painful and has no maximum degree of stiffness. Non-ischemic priapism requires timely assessment and attention, however, not being a compartment syndrome does not represent a medical urgency.
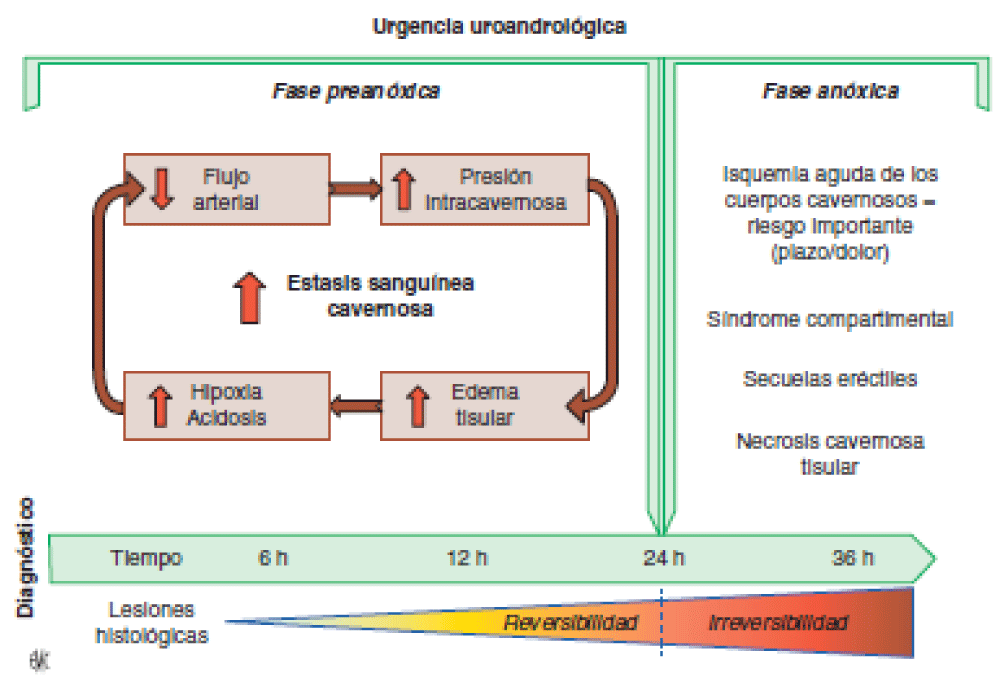
Figure 1:
One of the main causes of low-flow priapism is the use of drugs with α-adrenergic antagonist effect, among which antipsychotic drugs are highlighted and up to 50% of such cases are attributed to it. It is assumed that adrenergic blockage triggers an imbalance in favor of the parasympathetic tone with the resulting relaxation of the cavernous arterioles, decreased sinus venous return and persistent ingurgitation of caver-native bodies. Consequently, the increase in tissue pressure (which in practice constitutes a compartmental syndrome) comes to exceed blood pressure with the resulting ischemia, hypoxia and acidosis that, as the cascade of events progresses, will lead to thrombosis, cell death and penis fibrosis.
The widespread use of antipsychotics in medicine, psychiatry and other specialties obliges us to take into account this uncommon but harmful adverse event, which may well be cataloged as idiosyncratic because it does not relate to the dose of the psychopharmaceutical or the duration of treatment. We present and discuss an illustrative case.
23-year-old male, single, with an important history of mild autism, for which he has received regular treatment with 6 mg daily of risperidone. He started his priapism experience spontaneously for 4 days until he is taken by his family to the Emergency– intense, persistent, and painful penis erection. At the examination, he was patient without complaint of pain, with stable vital signs, and without other somatic alterations except for his notorious erection that respected the gland and the spongy body.
Among the auxiliary tests are hemoglobin 14.7g/dl, hematocrit 41% and leukocyte count 11.300 cells/mm3 (without left deviation), blood clotting tests, blood biochemistry, and urinalysis within normal limits. The aspirated blood from the cavernous bodies showed an unequivocal dark tint and its gasometry cast values of pH 6.97; pO2: 18.36 mmHg and pCO2: 85 mmHg.
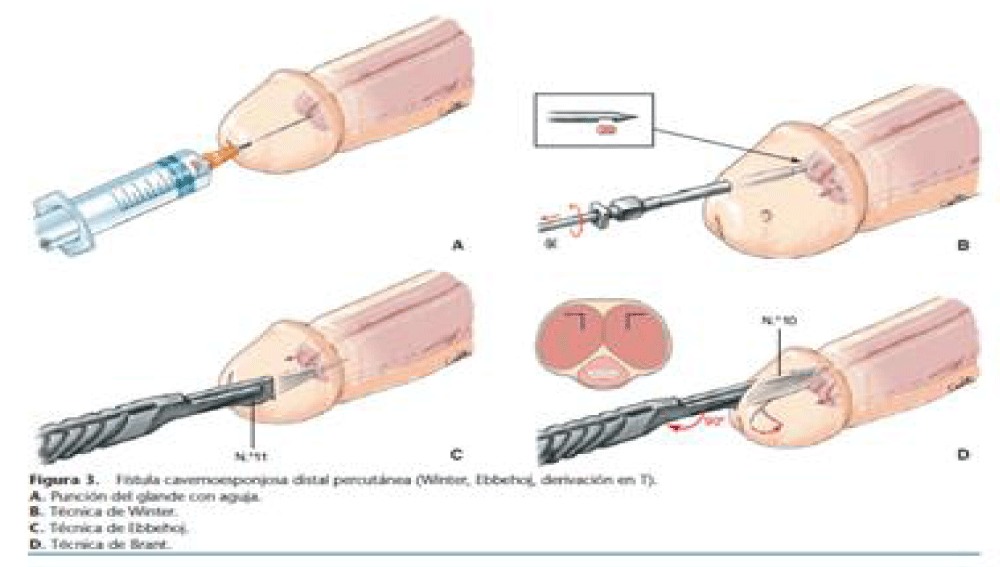
In the absence of other etiological factors, the case was diagnosed as low-flow priapism and the patient was provided with supporting measures (analgesia, sedation and hydration), as well as intracavernous injection of phenylephrine diluted in physiological saline solution (three applications of 0.5 mL each, at a concentration of 1 mg/mL). However, in the face of the failure of the medical treatment instituted, at 6 o’clock of evolution – the delay was due to no availability of a quirophan – it opted to practice a cavernous-spongy distal derivation (Winter’s surgical technique). With partial clinical improvement, Subsequently, at 36 h of observation, and not verifying adequate penile detumescence, the interrogation is contacted that the father in view of psychomotor agitation self-administers 3 mg of risperidone without prior notice to the doctor on duty which causes recurrence of clinical pain and tumescence, the decision was made to submit the patient to a second intervention, this time with the Ebbehoj technique (distal cavernous-spongy shunt): this time with the partially successful result with distal detumescence, having to repeat the technique with Brant modification (distal cavernous-spongy shunt) where there is a 90° rotation during the incision in the glans, performed on one occasion 24 hours after the previous procedure, with clinical improvement being able to discharge.
In the outpatient follow-up was recorded the spontaneous presence of nightly erections per month and at the three months of medical alert, our patient achieved the erection partially and although there is no reference to effectiveness when performing sexual intercourse. At present, after the described episode of priapism, the patient does not have erectile dysfunction and his psychotic picture is controlled with 450 mg daily of quetiapine [5,6].
Regarding the affinity of antipsychotics to the α1-adrenergic receptor, risperidone has an α1-antagonist capacity. In fact, the third cause of cases of priapism induced by atypical antipsychotics is secondary to risperidone, including recent cases associated with its parenteral presentation of deposit RisperdalConsta® – So far, cases inducted by the use of almost all second-generation antipsychotics, including aripiprazole, have been. Among other psychotropic drugs associated with the development of priapism, antidepressant and hypnotic trazodone is highlighted, with an incidence of up to one case for every thousand to ten thousand users. Even before the emergence of atypical antipsychotics, trazodone was responsible for 79% of cases of psycho-drug-induced priapism. Only rarely have other antidepressants been associated with priapism.
Recent reviews on the topic mention a four-hour limit of duration as a diagnostic criterion for priapism. Although globally the prognosis depends on the promptness of the intervention, even with the establishment of the specific treatment a high percentage of patients – between 50% and 90% – could develop total erectile dysfunction if priapism exceeds the 24 to 48 hours of duration since more time passed there will be less effectiveness of any intervention: this due to the abolition of the physiological mechanisms numbing and not by intrinsic failure, it is worth clarifying, of the medical or surgical procedures instituted. Although the population incidence of priapism is 1.5 per 100,000 (and doubles among men over 40 years old, which is the most affected age group).
The severity of the possible sequelae requires reinforcing the preventive attitude in the face of the possibility of this complication: in the case of priapism induced by antipsychotics, drugs commonly used chronically, an elementary preventive measure is to detect the presence of additional risk factors such as, among others: blood dyscrasias (polycythemia, thalassemia, sickle cell disease), consumption of psychoactive substances (alcohol, cocaine, amphetamines), use of other α-blocker drugs (terazosin, tamsulosin, guanethidine, etc.), which could discourage the use of antipsychotics with high α-antagonist affinity such as risperidone or, if prescribed, require close monitoring.
The therapeutic approach of priapism depends fundamentally on the type diagnosed: in the case of ischemic priapism, the initial management involves aspiration and direct irrigation of the cavernous bodies with diluted sympathetic agents – e.g., phenylephrine or ethylenimine – and, in the case of failure of these procedures, surgical anastomosis of the cavernous bodies into the spongy body or venous affluent – such as the major saphenous vein – must be performed in order to penile flaccidity: either anastomosis performed at the level of the gland or, in more severe cases, even at the base of the penis. The effectiveness of these procedures to preserve erectile function is not absolute, as has been mentioned.
Figure 2:
In the present case, we verify the unpredictability of priapism that depended on the prescribed dose of risperidone, at high doses, it is essential to consider the possibility of recurrence of Priapism and prevent it according to the risk factors involving, in the first place, the affinity of the antipsychotic chosen to the α1 blockage. Recurrence of priapism has been in cases of re-exposure to previously prescribed antipsychotics.
Based on the above, we emphasize the need to prevent priapism associated with antipsychotics, as far as possible, and the necessity of early urological intervention to avoid undesirable outcomes on the erectile capacity of our patients.
Regarding the affinity of antipsychotics to the α1-adrenergic receptor, risperidone has an α1-antagonist capacity. In fact, the third cause of cases of priapism induced by atypical antipsychotics is secondary to risperidone, including recent cases associated with its parenteral presentation of deposit RisperdalConsta® – So far, cases inducted by the use of almost all second-generation antipsychotics, including aripiprazole, have been. Among other psychotropic drugs associated with the development of priapism, antidepressant and hypnotic trazodone is highlighted, with an incidence of up to one case for every thousand to ten thousand users. Even before the emergence of atypical antipsychotics, trazodone was responsible for 79% of cases of psycho-drug-induced priapism. Only rarely have other antidepressants been associated with priapism.
Recent reviews on the topic mention a four-hour limit of duration as a diagnostic criterion for priapism. Although globally the prognosis depends on the promptness of the intervention, even with the establishment of the specific treatment a high percentage of patients – between 50% and 90% – could develop total erectile dysfunction if priapism exceeds the 24 to 48 hours of duration since more time passed there will be less effectiveness of any intervention: this due to the abolition of the physiological mechanisms numbing and not by intrinsic failure, it is worth clarifying, of the medical or surgical procedures instituted. Although the population incidence of priapism is 1.5 per 100,000 (and doubles among men over 40 years old, which is the most affected age group).
The severity of the possible sequelae requires reinforcing the preventive attitude in the face of the possibility of this complication: in the case of priapism induced by antipsychotics, drugs commonly used chronically, an elementary preventive measure is to detect the presence of additional risk factors such as, among others: blood dyscrasias (polycythemia, thalassemia, sickle cell disease), consumption of psychoactive substances (alcohol, cocaine, amphetamines), use of other α-blocker drugs (terazosin, tamsulosin, guanethidine, etc.), which could discourage the use of antipsychotics with high α-antagonist affinity such as risperidone or, if prescribed, require close monitoring.
The therapeutic approach of priapism depends fundamentally on the type diagnosed: in the case of ischemic priapism, the initial management involves aspiration and direct irrigation of the cavernous bodies with diluted sympathetic agents – e.g., phenylephrine or ethylenimine – and, in the case of failure of these procedures, surgical anastomosis of the cavernous bodies into the spongy body or venous affluent – such as the major saphenous vein – must be performed in order to penile flaccidity: either anastomosis performed at the level of the gland or, in more severe cases, even at the base of the penis. The effectiveness of these procedures to preserve erectile function is not absolute, as has been mentioned.
In the present case, we verify the unpredictability of priapism that depended on the prescribed dose of risperidone, at high doses, it is essential to consider the possibility of recurrence of Priapism and prevent it according to the risk factors involving, in the first place, the affinity of the antipsychotic chosen to the α1 blockage. Recurrence of priapism has been in cases of re-exposure to previously prescribed antipsychotics.
Based on the above, we emphasize the need to prevent priapism associated with antipsychotics, as far as possible, and the necessity of early urological intervention to avoid undesirable outcomes on the erectile capacity of our patients.
- Broderick GA, Kadioglu A, Bivalacqua TJ, Ghanem H, Nehra A, Shamloul R. Priapism: pathogenesis, epidemiology, and management. J Sex Med. 2010 Jan;7(1 Pt 2):476-500. doi: 10.1111/j.1743-6109.2009.01625.x. PMID: 20092449.
- Burnett AL, Bivalacqua TJ. Priapism: new concepts in medical and surgical management. Urol Clin North Am. 2011 May;38(2):185-94. doi: 10.1016/j.ucl.2011.02.005. PMID: 21621085.
- Compton MT, Miller AH. Priapism associated with conventional and atypical antipsychotic medications: a review. J Clin Psychiatry. 2001 May;62(5):362-6. doi: 10.4088/jcp.v62n0510. PMID: 11411819.
- Kadioglu A, Sanli O, Celtik M, Cakan M, Taskapu H, Akman T. Practical management of patients with priapism. EAU-EBU update series. 2006; 4: 150-60.
- Sood S, James W, Bailon MJ. Priapism associated with atypical antipsychotic medications: a review. Int Clin Psychopharmacol. 2008 Jan;23(1):9-17. doi: 10.1097/YIC.0b013e3282f1c1ef. PMID: 18090503.
- Makesar D, Thome J. Risperidone-induced priapism. World J Biol Psychiatry. 2007;8(1):45-7. doi: 10.1080/15622970600797575. PMID: 17366350.