More Information
Submitted: April 24, 2023 | Approved: May 04, 2023 | Published: May 05, 2023
How to cite this article: Alijanzadeh D, Arabpour E, Abdi M, Abdehagh M. An uncommon gastrointestinal bleeding in a patient with portal vein thrombosis: a case report and literature review. Arch Case Rep. 2023; 7: 015-019.
DOI: 10.29328/journal.acr.1001069
Copyright License: © 2023 Alijanzadeh D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Portal vein thrombosis; Upper gastrointestinal bleeding; Coffee ground emesis; GIB
An uncommon gastrointestinal bleeding in a patient with portal vein thrombosis: a case report and literature review
Dorsa Alijanzadeh1, Erfan Arabpour2* , Mohammadamin Abdi1 and Mohammad Abdehagh2*
, Mohammadamin Abdi1 and Mohammad Abdehagh2*
1Department of Internal Medicine, Imam Hossein Hospital, Shahid Beheshti University
of Medical Sciences, Tehran, Iran
2Department of Gastroenterology and Hepatology, Imam Hossein Hospital, Shahid
Beheshti University of Medical Sciences, Tehran, Iran
*Address for Correspondence: Erfan Arabpour, MD, Department of
Gastroenterology and Hepatology, Imam Hossein Hospital, Shahid Beheshti University of Medical
Sciences, SBUMS, Arabi Ave, Daneshjoo Blvd, Velenjak, Tehran, Iran, Email:
[email protected]
Mohammad Abdehagh, MD, Department of Gastroenterology and Hepatology, Imam Hossein Hospital,
Shahid Beheshti University of Medical Sciences, SBUMS, Arabi Ave, Daneshjoo Blvd, Velenjak,
Tehran, Iran, Email: [email protected]
Portal vein thrombosis (PVT) is a rare condition that may congest bowel venous drainage and cause mesenteric ischemia. In acute settings, gastrointestinal bleeding (GIB) is rare, and acute abdominal pain is the most common clinical presentation. A 24-year-old man who presented with acute abdominal pain and a single episode of hematemesis is reported. Workups revealed evidence of thrombosis in the portal vein, but upper endoscopy was incapable to detect the source of the bleeding. We discuss the possible scenarios for the GIB in this case and review similar reports in the literature.
Portal vein thrombosis (PVT) is a rare condition that may congest bowel venous drainage and cause mesenteric ischemia. Liver cirrhosis accounts for about 85% of PVTs [1].
In chronic settings, esophageal varices hemorrhage due to portal hypertension is the most likely mechanism which presents as hematemesis, melena, or hematochezia. On the other hand, in acute settings, gastrointestinal bleeding (GIB) is rare, and acute abdominal pain is the most common clinical presentation [2,3].
Obscure GIB is defined as bleeding from an unknown source after unremarkable diagnostic evaluations. An overwhelming majority of patients with obscure GIB present with melena or hematochezia; hematemesis is rare [4].
Here we present a case of acute PVT with obscure upper GIB through the upper endoscopy and review the suggested mechanisms and previous reports.
A 24-year-old Persian male with a non-significant past medical history arrived at the emergency department (ED) with a chief complaint of a single episode of bloody vomiting. The patient had been experiencing abdominal pain two days before visiting the ED. The pain had started suddenly in the morning, was 10/10 in intensity, located in the epigastric and left upper quadrant regions, non-radiating, and did not alter by meal, activity, or rest; yet he did not seek any medical care. On the morning of arriving at the ED (the third day), the patient vomited two cups of dark red blood without any food particles. He had had non-bloody diarrhea for the past two days which had resolved by the time of the presentation to ED. He denied any fever, shortness of breath, previous gastrointestinal disorders, recent abdominal trauma, alcohol use, and smoking. He had taken over-the-counter painkillers (Non-steroidal anti-inflammatory drug (NSAID)) for the past two days and denied taking other medications, herbals, and drugs of abuse. He denied any clotting disorders in his family. In the physical examination, he was a young ill-appearing man, with vital signs: blood pressure of 130/80 mmHg, pulse rate of 88 beats per minute, respiratory rate of 18 per minute, and was afebrile. His abdomen appeared mildly distended on inspection. It was soft on palpation but tender in the epigastric region without rebound tenderness. The digital rectal exam was fecal and non-bloody. Cardiovascular, respiratory, and neurological examination findings were within normal limits.
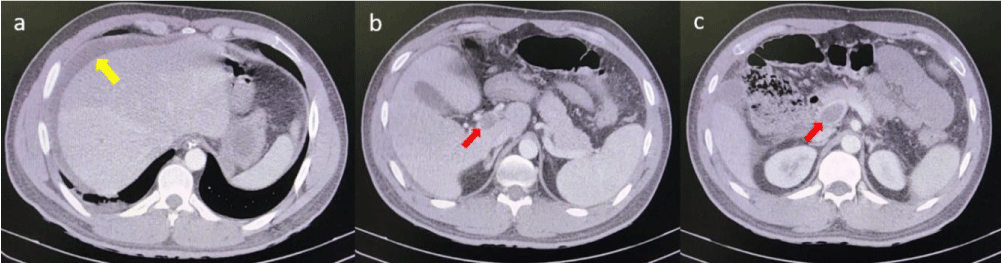
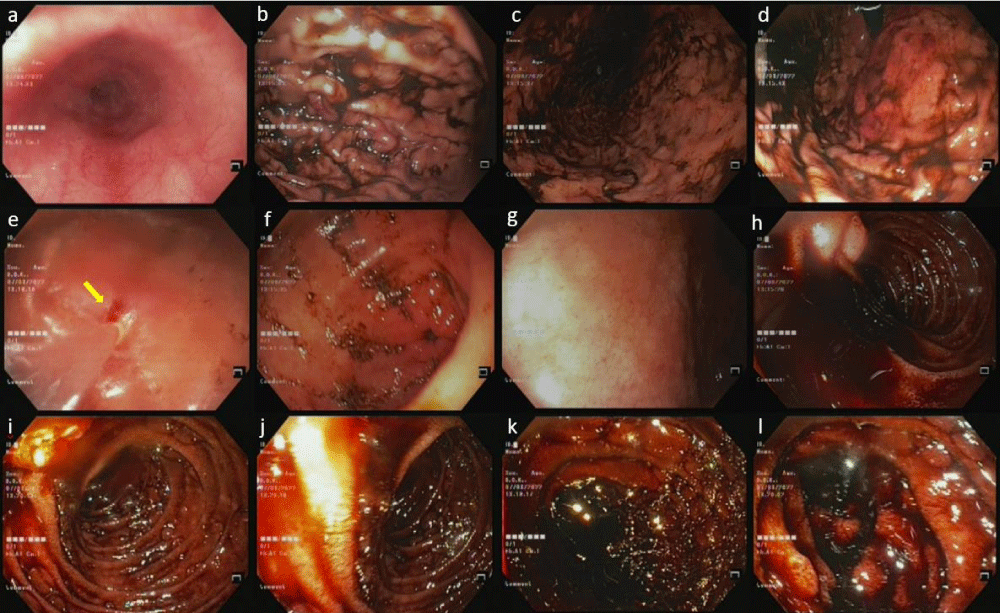
The laboratory workups on admission are presented in Table 1. Contrast-enhanced CT scan of the abdomen and pelvis revealed evidence of thrombosis in the portal and superior mesenteric veins (Figure 1). Nasogastric tube (NGT) insertion aspirated almost 100cc of coffee ground secretions. Before initiating anticoagulant therapy, the patient had undergone upper endoscopy for GIB diagnostic workup. In the endoscopy, the esophagus was normal, without any evidence of esophageal varices. Coffee-ground blood was seen on the fundus, body, and antrum of the stomach. The Mucosa of the antrum was congested; however, no significant lesion was noted on the gastric mucosa. No fundal varices were seen in the retroversion maneuver. The distal part of the duodenum was full of coffee ground blood but no prominent lesion was noted in the duodenum. Upper endoscopy did not detect the source of the bleeding, but a suspicious oozing of coffee-ground blood from the duodenal papilla was reported by the endoscopist (Figure 2). Anticoagulant therapy with heparin was initiated for the patient.
| Table 1: A brief summary of laboratory workup on admission. | |||
| Laboratory test | Results | Reference range | |
| White blood cell (WBC) | 14.7 H | 4.4 – 11.2 (*103/µL) | |
| Hemoglobin (Hb) | 15.9 | 12- 16 (g/dL) | |
| Platelet (Plt) | 132 L | 150 – 450 (*103/µL) | |
| C reactive protein (CRP) | 14.6 H | Up to 5.9 (mg/L) | |
| Lactate dehydrogenase (LDH) | 593 H | 230 – 480 (U/L) | |
| Blood urea nitrogen (BUN) | 22.9 | 15 – 45 (mg/dL) | |
| Creatinine (Cr) | 1.3 | 0.5 – 1.5 (mg/dL) | |
| Sodium (Na) | 137 | 133 – 146 (mmol/L) | |
| Potassium (K) | 4.7 | 3.8 – 5 (mmol/L) | |
| Blood sugar (BS) | 154 H | Up to 140 (mg/dL) | |
| Prothrombin time (PT) | 15.1 H | 10.0 – 13.6 (s) | |
| Partial thromboplastin time (PTT) | 20.6 | 20 – 40 (s) | |
| Aspartate aminotransferase (AST) | 24 | 5 – 38 (U/L) | |
| Alanine aminotransferase (ALT) | 31 | 5 – 42 (U/L) | |
| Alkaline phosphatase (ALP) | 157 | 80 – 306 (U/L) | |
| Amylase | 38 | Up to 90 (U/L) | |
| Lipase | 17 | Up to 60 (U/L) | |
| Total bilirubin | 1.95 H | 0.5 – 1.5 (mg/dL) | |
| Direct bilirubin | 0.6 H | Up to 0.5 (mg/dL) | |
| SARS-Cov-2 PCR | RDRP | Was not detected | - |
| E. gene | Was not detected | - | |
| Venous Blood Gas (VBG) | pH | 7.44 H | 7.31 – 7.41 |
| pCO2 | 44.6 | 40 – 52 (mmHg) | |
| HCO3- | 29.4 H | 22 – 27 (mmol/L) | |
Figure 1: Anteroposterior (AP) radiograph of both hands and Anteroposterior (AP) radiography of pelvis.
Figure 2: (a) Esophagus; (b) body of stomach; (c), (d) Fundus; (e) Erythematous line on lesser curvature (yellow arrow); (f) Antrum; (g) bulb of duodenum; (h), (i), (j) Duodenal papilla and a suspicious bleeding from it; (k), (l) Distal duodenum.
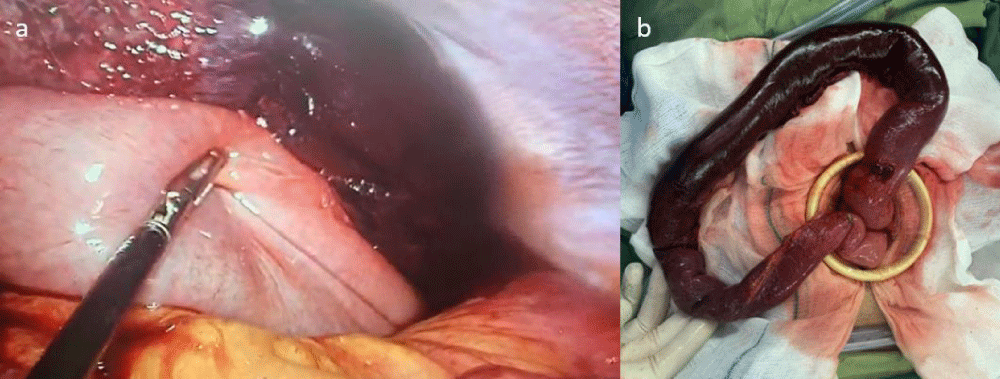
In consultation with the interventional radiologist over possible embolectomy, the radiologist strongly recommended performing an emergency laparotomy. At first, the patient was reluctant to undergo surgery, but lastly, he agreed and after about 30 hours from the time of referral, he underwent a diagnostic laparoscopic surgery. In the laparoscopy, after suctioning large amounts of serous fluid in the abdomen, the first 60 cm of the proximal part of the jejunum was gangrenous. The operation plan was changed to laparotomy and the gangrenous section was resected and a side-to-side anastomosis was performed (Figure 3). Eight days after the surgery, the patient was discharged with apixaban 5 mg twice daily and was given a follow-up appointment while repeating the abdominal imaging. Further laboratory workups revealed hyperhomocysteinemia, then folic acid, vitamin B6, and vitamin B12 were added to the treatment regimen (Tables 2,3).
| Table 2: A brief summary of laboratory findings in the patients. | |||
| Laboratory test | Results | Reference range | |
| Inpatient | After discharge | ||
| Cardiolipin Ab IgG | < 3.0 | 1.9 | Non-reactive: < 10, Equivocal: 10 – 12, Reactive: >12 (U/mL) |
| Cardiolipin Ab IgM | < 3.0 | 1.4 | Negative: < 12, Equivocal: 12 – 18, Positive: > 18 (U/mL) |
| Phospholipid Ab IgG | 0.40 | 0.30 | Negative: < 0.9, Borderline: 0.9 – 1.1, Positive: > 1.1 (Ratio) |
| Phospholipid Ab IgM | 0.2 | 0.2 | Negative: < 0.9, Borderline: 0.9 – 1.1, Positive: > 1.1 (Au/mL) |
| Beta-2 Glycoprotein IgG | 1.2 | 1.6 | Negative: < 12, Equivocal: 12 – 18, Positive: > 18 (Au/mL) |
| Beta-2 Glycoprotein IgM | 2.5 | 1.4 | Negative: < 12, Equivocal: 12 – 18, Positive: > 18 (Au/mL) |
| Anti-ds-DNA | 11.3 | 11.3 | Negative: Up to 30, Equivocal: 30 – 35, Positive: > 35 (IU/mL) |
| P-ANCA | 8.0 | 8.5 | Negative: < 12, Equivocal: 12 – 18, Positive: > 18 (U/mL) |
| C-ANCA | 7.6 | 7.2 | Negative: < 12, Equivocal: 12 – 18, Positive: > 18 (U/mL) |
| ANA | < 1/100 | < 1/100 | Up to 1/100 (titer) |
| C3 | 151.0 | 96.3 | 90 - 180 (mg/dL) |
| C4 | 25.2 | 31.3 | 10 – 40 (mg/dL) |
| CH50 | 78.00 | 82.90 | 41.68 – 95.06 (mg/dL) |
| Lupus anticoagulant | Negative | Negative | negative |
| Homocysteine | - | 77.5 H | 5.0 – 15.0 (µmol/L) |
| Assay FV | - | 86 | % (more than 70) |
| Protein S | - | 67 | % (more than 65) |
| Protein C | - | 60 L | % (more than 70) |
| Anti-thrombin III | 107 | % (more than 70) | |
| Table 3: Similar reports of gangrenous jejunum as responsible for upper GIB. | |||||||||
| References | Demographic data | Clinical presentation | Thrombosis diagnostic method | Thrombosis location | Endoscopic findings | Source of bleeding | Management | Etiology | Outcome |
| [6] | Male, 77 years old | Abdominal pain, blood-stained diarrhea, the Coffee ground vomiting | Abdominopelvic CT scan | Thrombotic occlusion in SMV extending to the proximal part of the portal vein | Not mentioned | 120 cm gangrenous part started from treitz ligament | Laparotomy | Not mentioned | Discharged |
| [7] | Male,13 years old | Colicky abdominal pain, hematemesis, melena | Abdominal CT scan with and without contrast | Right and left branches of the portal vein, SMV, and hepatic veins | Fresh blood coming from the jejunum | 25 cm gangrenous part of proximal jejunum | Laparotomy | Eosinophilic mesentric vasculitis | Discharged |
| CT: Computed Tomography; SMV: Superior Mesenteric Vein | |||||||||
Figure 3: Gangrenous jejunum in (a) diagnostic laparascopy and (b) open laparotomy.
We presented a case of PVT with upper GIB of an unknown source. Hematemesis (upper GIB) suggests bleeding proximal to the treitz ligaments. In patients with PVT, esophageal varices are the leading cause of hematemesis; gastric ischemia is a rare cause [5]. In this case, upper endoscopy reported coffee ground secretions in the stomach and duodenum but no source was suggested. We discuss the possible scenarios for the GIB in this case as follows:
I) Gangrenous jejunum
In laparoscopy, the jejunum was gangrenous in the section exactly distal to the treitz ligament. In the upper endoscopy, no obvious source was found for the bleeding, but the distal part of the duodenum was full of coffee ground secretions. The patient was hemodynamically stable and the tilt test was negative on admission. Baseline hemoglobin was 15.9 g/dl and no reduction in hemoglobin was observed during serial Complete blood counts (CBCs). Putting all these together, the most likely hypothesis is that the source of hematemesis was necrotizing particles of gangrenous jejunum. In the literature review, Ahmad, et al. reported a similar case; a patient with abdominal pain and coffee ground emesis which eventually infarcted jejunum was diagnosed as the source of upper GIB. However, they did not perform an upper endoscopy to rule out other possible sources [6]. Another case of gangrenous jejunum as the culprit of upper GIB was reported by Abdulwahab, et al.; a 13 years old boy with hematemesis which the upper endoscopy revealed active bleeding originating from a gangrenous jejunum due to PVT [7].
II) Oozing bleeding from duodenal papilla
A suspicious oozing bleeding through the duodenal papilla was reported in upper endoscopy. AST, ALT, ALP, amylase, and lipase were within normal limits and no sign of infarct or inflammation of the pancreaticobiliary system was seen in the CT scan. Therefore, imaging and laboratory investigation results make bleeding from the duodenal papilla unlikely; suggesting that the observed secretions were probably dark bile.
III) Peptic ulcer disease due to the NSAIDs
There was a history of taking oral NSAIDs for abdominal pain two days before the hematemesis. In the upper endoscopy, a small erythematous line was observed on the lesser curvature of the stomach, which seemed to be caused by the NG-tube insertion; no ulcer was seen in the stomach and duodenum. Thus, this hypothesis seems improbable.
Putting all the patient’s history, laboratory workups, imaging, and diagnostic laparoscopy findings together, the most plausible hypothesis is that the bleeding originated from the gangrenous jejunum. However, hematemesis originating distal to the treitz ligament is unlikely and there are only a few reports of it.
Bou-Abdallah, et al. reviewed six cases of coffee ground emesis who had an overlooked disorder due to preoccupation with the GIB. Although these patients were admitted for upper GIB, the more significant associated diagnosis included bilateral pulmonary emboli, acute myocardial infarction, urosepsis, small bowel obstruction and acute renal failure; all were hemodynamically stable with no fall in hemoglobin/hematocrit [8]. Just like this patient, who visited with a complaint of coffee ground emesis and was hemodynamically stable with normal hemoglobin, and was diagnosed with PVT. Coffee ground emesis etiology is not limited to the gastrointestinal tract and patients may require a comprehensive diagnostic workup.
Inpatient routine laboratory workups were unremarkable for the etiology of the thrombosis. There was no history of clotting disorders in his family. During the COVID-19 pandemic, many cases of thromboembolism caused by COVID-19 infection or vaccination were reported [9]. The two polymerase chain reaction (PCR) tests for COVID-19 during hospitalization were negative. The patient denied any recent fever, fatigue, malaise, dyspnea, and other symptoms of any infection. He had received three doses of the BBIBP-CorV (Sinopharm™) vaccine, and six months passed since the last dose. A systematic review of cases of PVT caused by COVID-19 reported that PVT usually occurs within two weeks after vaccination, and is more common after the first dose [10]. Thus, an association between COVID-19 and thrombosis in this patient seems unlikely. Further outpatient investigation revealed hyperhomocysteinemia and a low level of protein C.
Here we reported an unusual presentation of a PVT with an uncommon source for the GIB. Although hematemesis suggests bleeding proximal to the treitz ligaments, in rare cases, the source of bleeding may be in the proximal part of the jejunum. The most reasonable hypothesis seems to be that the bleeding originated from the gangrenous jejunum. However, hematemesis originating distal to the treitz ligament is unlikely and there are only a few reports of it. A push enteroscopy and an analysis of the secretions could help resolve this mystery.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
We would like to express our appreciation to Dr. Iranshahi and Dr. Samsami for their practical suggestions.
- Mantaka A, Augoustaki A, Kouroumalis EA, Samonakis DN. Portal vein thrombosis in cirrhosis: diagnosis, natural history, and therapeutic challenges. Ann Gastroenterol. 2018 May-Jun;31(3):315-329. doi: 10.20524/aog.2018.0245. Epub 2018 Mar 3. PMID: 29720857; PMCID: PMC5924854.
- Ponziani FR, Zocco MA, Campanale C, Rinninella E, Tortora A, Di Maurizio L, Bombardieri G, De Cristofaro R, De Gaetano AM, Landolfi R, Gasbarrini A. Portal vein thrombosis: insight into physiopathology, diagnosis, and treatment. World J Gastroenterol. 2010 Jan 14;16(2):143-55. doi: 10.3748/wjg.v16.i2.143. PMID: 20066733; PMCID: PMC2806552.
- Samant H, Asafo-Agyei KO, Garfield K. Portal vein thrombosis. In StatPearls [Internet]: StatPearls Publishing. 2021.
- Awadie H, Zoabi A, Gralnek IM. Obscure-overt gastrointestinal bleeding: a review. Pol Arch Intern Med. 2022 May 30;132(5):16253. doi: 10.20452/pamw.16253. Epub 2022 May 30. PMID: 35635400.
- Alzubaidi S, Patel I, Saini A, Knuttinen G, Naidu S, Kriegshuaser S, Albadawi H, Oklu R. Current concepts in portal vein thrombosis: etiology, clinical presentation and management. Abdom Radiol (NY). 2019 Oct;44(10):3453-3462. doi: 10.1007/s00261-019-02174-1. PMID: 31407054.
- Ahmad MSM, Iqbal MR, Refson JS. Acute mesenteric ischaemia due to superior mesenteric vein (SMV) thrombosis. BMJ Case Rep. 2021 Apr 1;14(4):e239110. doi: 10.1136/bcr-2020-239110. PMID: 33795268; PMCID: PMC8021585.
- Abdulwahab A, Almoallim H, Khan N. Isolated eosinophilic mesenteric vasculitis with extensive thrombosis and splenic infarction in a 13-year-old boy. Clin Rheumatol. 2007 Feb;26(2):254-7. doi: 10.1007/s10067-005-0128-7. Epub 2005 Dec 7. PMID: 16333561.
- Bou-Abdallah JZ, Murthy UK, Mehta N, Prasad HN, Kaul V. Coffee grounds emesis: not just an upper GI bleed. J Emerg Med. 2012 Jul;43(1):44-6. doi: 10.1016/j.jemermed.2009.05.008. Epub 2009 Jun 28. PMID: 19564091.
- Malas MB, Naazie IN, Elsayed N, Mathlouthi A, Marmor R, Clary B. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: A systematic review and meta-analysis. EClinicalMedicine. 2020 Dec;29:100639. doi: 10.1016/j.eclinm.2020.100639. Epub 2020 Nov 20. PMID: 33251499; PMCID: PMC7679115.
- Kheyrandish S, Rastgar A, Arab-Zozani M, Sarab GA. Portal Vein Thrombosis Might Develop by COVID-19 Infection or Vaccination: A Systematic Review of Case-Report Studies. Front Med (Lausanne). 2021 Dec 14;8:794599. doi: 10.3389/fmed.2021.794599. PMID: 34970570; PMCID: PMC8712467.