More Information
Submitted: March 29, 2023 | Approved: April 14, 2023 | Published: April 17, 2023
How to cite this article: Mohammad N, Pouya H, Leila A, Ali MM, Mazyar B, et al. Osteopoikilosis: a rare case with interesting imaging. Arch Case Rep. 2023; 7: 012-014.
DOI: 10.29328/journal.acr.1001068
Copyright License: © 2023 Mohammad N, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Osteopoikilosis; Bone scintigraphy; X-ray imaging
Osteopoikilosis: a rare case with interesting imaging
Nejadhosseinian Mohammad1,2, Hadighi Pouya1, Aghaghazvini
Leila3, Mozaffari Mohammad Ali4, Babagoli Mazyar2* and Faezi Seyedeh Tahereh2
and Faezi Seyedeh Tahereh2
1Joint Reconstruction Research Center, Tehran University of Medical Science,
Tehran, Iran
2Rheumatology Research Center (RRC), Dr. Shariati Hospital, Kargar Avenue, Tehran
University of Medical Sciences, Tehran 14117-13137, Iran
3Department of Radiology, Shariati Hospital, Tehran University of Medical Sciences,
Tehran, Iran
4Division of Plastic Surgery, Yale School of Medicine, New Haven, CT, USA
*Address for Correspondence: Babagoli Mazyar, Rheumatology Research Center (RRC), Dr. Shariati Hospital, Kargar Avenue, Tehran University of Medical Sciences, Tehran 14117-13137, Iran, Email: [email protected]
Background: Osteopoikilosis (OPK) is a rare osteosclerotic dysplasia. It is usually asymptomatic and diagnosis is made incidentally by radiographic findings. It has a unique radiographic presentation with multiple small, well-defined, circular, or ovoid radiodensities which are distributed symmetrically in the epiphysis and metaphysis of long bones.
Aim of the work: In this case report, a 38-year-old man with mild joint discomfort was diagnosed with OPK according to his radiographic findings and literature review.
Conclusion: It is important to diagnose OPK and to distinguish it from other medical conditions to calm the patient and to reduce unnecessary investigation.
Osteopoikilosis is a rare form of skeletal abnormality. The condition is a type of bone sclerosing dysplasia that is usually asymptomatic; diagnosis is made by incidental radiological findings in patients seeking treatment for other medical disorders such as fractures. Osteopoikilosis follows an autosomal dominant distribution pattern with some cases happening sporadically. The typical radiographic finding in osteopoikilosis is, small, well-defined, circular, or ovoid radiodensities which are distributed symmetrically in the epiphysis and metaphysis of long bones. In histology, these sclerotic lesions appear as bony islands in cancellous bone. Patients are usually diagnosed between the ages of 15 to 60 but there is no age or sex preponderance [1-3]. Abnormality in the endochondral bone maturation process and collagen regulation is the main pathogenesis of this condition which is caused by a mutation in the LEMD3 gene [4]. Association of connective tissue nevi (dermatofibrosis lenticularis dissemina) with typical sclerotic bone lesions of osteopoikilosis are seen in the same rare cases known as Buschke-Ollendorff syndrome [5]. The goal of diagnosing osteopoikilosis is to separate it from more serious conditions such as osteoblastic metastasis.
A 38- year -old man presented at the rheumatology clinic of Shariati Hospital with the chief complaint of mild discomfort in the left wrist since 6 years ago. In addition, he had a new onset of mild discomfort at both ankles and pelvic areas. He had a past medical history of mild chronic kidney disease with increased serum creatinine level and increased cortical echogenicity in ultra-sonography of both kidneys. In physical examination, there was no swelling or tenderness on both wrists, ankles, or hips. The range of motion of both wrists, ankles, and hips was normal. Examination of other joints and spinal column were normal. No other clue was found in his history and physical examination.
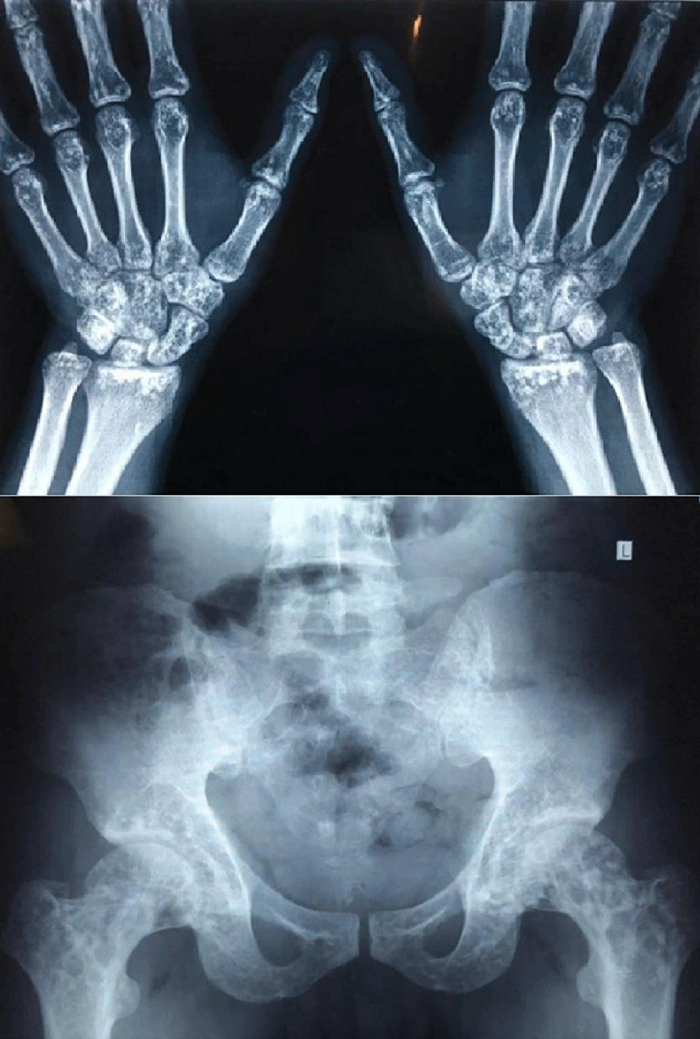
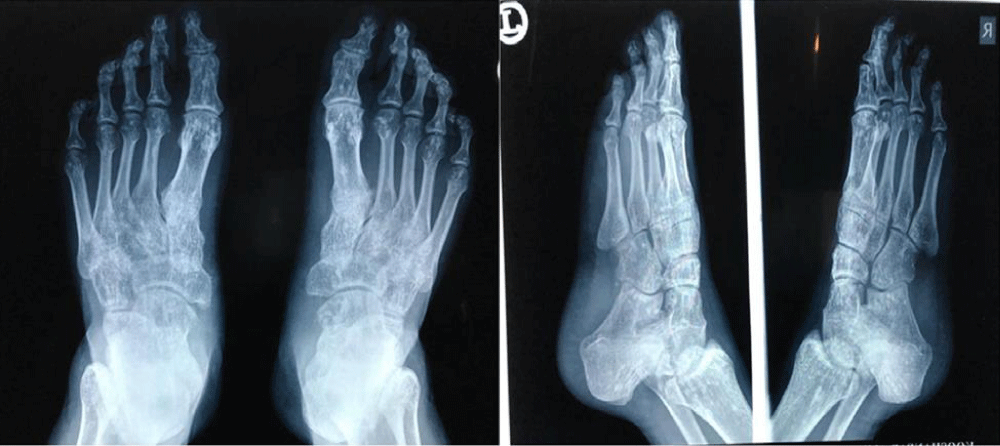
X-ray studies of feet, ankles, hands, wrists, and pelvis revealed the existence of multifocal clusters of small, round to oval, well-defined border, sclerotic lesions located along the proximal and distal epiphysis of joints, at bilateral tarsal joints in lisfranc and Chopart, MTP (metatarsophalangeal), PIP (proximal interphalangeal), DIP (distal interphalangeal) of both feet, both hips, wrists, MCP (metacarpophalangeal), PIP and DIP joints of both hands. The morphology of these lesions noticed on X-rays was identical to those seen in osteopoikilosis. All bones were free of any cortical erosion or periosteal reaction (Figures 1,2).
Figure 1: Anteroposterior (AP) radiograph of both hands and Anteroposterior (AP) radiography of pelvis.
Figure 2: Anteroposterior (AP) and Oblique view radiography of both feet.
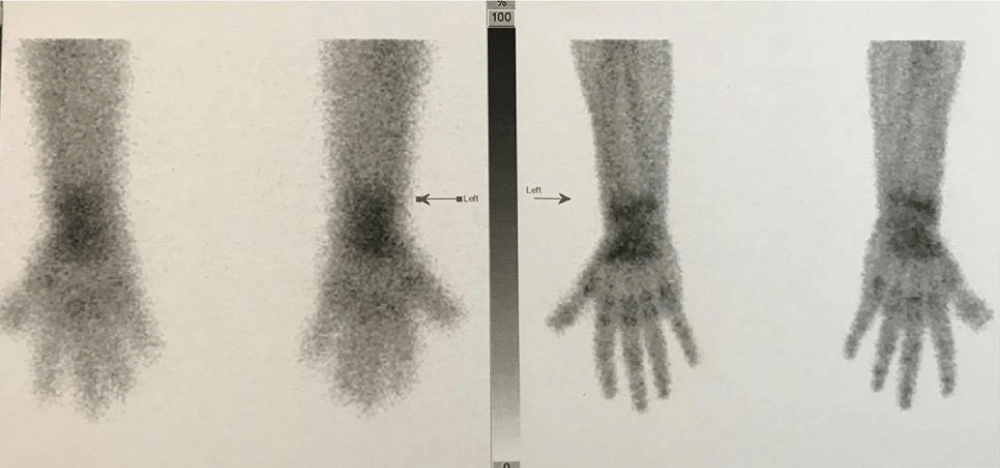
Three-phase bone scintigraphy showed a mild increase in radiotracer uptake in the left wrist but no focal radiotracer uptake in the left wrist and other sites of the body. Examination of other joints and spinal column were normal (Figure 3).
Figure 3: Three-phase bone scintigraphy of both hands.
Laboratory tests such as routine cell blood counts, erythrocyte sedimentation rate [ESR], serum electrolytes, urine analysis, thyroid function tests, alkaline phosphatase, liver function tests, rheumatoid factor [RF], antinuclear antibody [ANA] and anti-dsDNA were negative.
After confirming that there is no underlying malignancy or inflammatory disease, Osteopoikilosiss was the only suitable diagnosis for him. He was discharged with acetaminophen.
Osteopoikilosis is a rare and benign sclerosing dysplasia of bone characterized by the presence of numerous bone islands in the skeleton. Incidence is approximately 1 in 50000. Patients are usually diagnosed between the ages of 15 to 60 but there is no age or sex preponderance [1-3].
Although the pathogenesis and etiology of osteopoikilosis are still unclear, studies show that the LEMD3 gene is responsible for cases with autosomal dominant distribution pattern. LEMD3 can antagonize both the s Bone morphogenetic protein (BMP) and Transforming growth factor beta (TGF-β) signaling pathway resulting in hyperostotic bone disorders [4,6]. These lesions are made of dense trabeculae of spongious bone, sometimes forming a nidus that has no communication with bone marrow [7,8].
Osteopoikilosis is usually asymptomatic. Patients usually seek medical care for conditions not directly related to Osteopoikilosis. Therefore, OP is usually considered a chance finding. Joint pain and swelling are the main clinical feature in 20% of patients [9]. Association of small yellow papules and plaques, which are connective tissue nevi in osteopoikilosis patients is known as Buschke-Ollendorff syndrome [9].
Diagnosis is based on radiologic findings. A bone scan is sometimes used to distinguish osteopoikilosis from malignant metastasis. Osteopoikilosis is described by several 2 mm - 10 mm, round to oval, radio-opaque densities in cancellous bone tissue within epiphyses and metaphyses of long bones with a symmetric distribution pattern [1-3]. The most common sites are phalanges (100%), carpal bones (97.4%), metacarpals (92.3%), foot phalanges (87.2%), metatarsal (84.4%), tarsal (84.6%), pelvis (74.4%), femur (74.4%), radius (66.7%), ulna (66.7%) and tibia (20.5%) and is less common in ribs, vertebrae and skull [3]. The pattern of these sclerotic lesions may be related intimately to mechanical strain on cancellous bone trabeculae [3,10]. In the bone scan, due to active osseous remodeling, slightly increased activity is present [9]. However, an abnormal bone scan doesn’t exclude osteopoikilosis if typical radiologic findings are present [11].
Differential diagnosis includes osteoblastic metastasis, mastocytosis, synovial chondromatosis, tuberous sclerosis, Paget’s disease, osteopathia striata, melorheostosis and Ollier’s disease [8].
Among these disorders, osteoblastic metastasis is the most critical one to distinguish from osteopoikilosis. In Osteopoikilosis, lesions are symmetrical and uniform in size and follow a periarticular distribution. In OPK patients, bone scan is normal or slightly increased activity, and alkaline and acid phosphatase level is in the normal range. In contrast, asymmetry, axial skeleton involvement, bony destruction, and positive bone scan are the main diagnostic features of osteoblastic metastasis [1,3,10].
No specific treatment or further investigations is needed due to the benign course of the disease. Patient education and reassurance is the key to patient management [12]. Non-steroidal anti-inflammatory drugs [NSAIDs], acetaminophen, and opioids can be to relieve pain. Rare active lesions have been treated with bisphosphonate therapy, but the results are controversial [13].
Complications of osteopoikilosis are rare, but cases of osteosarcoma, chondrosarcoma, and giant cell tumor have been reported although no definite association has been established [3].
Osteopoikilosis is a rare disease. The importance of diagnosing this disease is to distinguish it from much more important medical conditions such as osteoblastic metastasis to prevent unnecessary investigation and decrease the level of anxiety and fear in patients.
Authors’ contributions
MN and PH contributed in data gathering. LA interpreted imaging. MM and MM contributed in writing the manuscript. FT was the main physician and analysed data. The final version of manuscript was approved by all authors.
Statements
Availability of data and materials: All data generated or analyzed during this study are included in this published article.
Ethics approval statement: The ethics committee of Tehran University of Medical Sciences, Tehran, Iran, has approved this manuscript.
Patient consent statement: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Declaration: The authors of this manuscript are not representatives of the government, and this paper is not submitted on behalf of any government department or organization.
- Khot R. Osteopoikilosis: A case report. Indian Journal of Radiology and Imaging. 2005; 15(4): 453-454.
- Paraskevas G, Raikos A, Stavrakas M, Spanidou S, Papaziogas B. Osteopoikilosis: a case report of a symptomatic patient. J Radiol Case Rep. 2009;3(12):38-43. doi: 10.3941/jrcr.v3i12.260. Epub 2009 Dec 1. PMID: 22470634; PMCID: PMC3303288.
- Krishna D, Chand S. Osteopoikilosis: A case report with review of literature. Journal of Orthopedics, Traumatology and Rehabilitation. 2013; 6(1): 84.
- Baasanjav S, Jamsheer A, Kolanczyk M, Horn D, Latos T, Hoffmann K, Latos-Bielenska A, Mundlos S. Osteopoikilosis and multiple exostoses caused by novel mutations in LEMD3 and EXT1 genes respectively--coincidence within one family. BMC Med Genet. 2010 Jul 9;11:110. doi: 10.1186/1471-2350-11-110. PMID: 20618940; PMCID: PMC2912259.
- Roberts NM, Langtry JA, Branfoot AC, Gleeson J, Staughton RC. Case report: osteopoikilosis and the Buschke-Ollendorff syndrome. Br J Radiol. 1993 May;66(785):468-70. doi: 10.1259/0007-1285-66-785-468. PMID: 8391368.
- Hellemans J, Preobrazhenska O, Willaert A, Debeer P, Verdonk PC, Costa T, Janssens K, Menten B, Van Roy N, Vermeulen SJ, Savarirayan R, Van Hul W, Vanhoenacker F, Huylebroeck D, De Paepe A, Naeyaert JM, Vandesompele J, Speleman F, Verschueren K, Coucke PJ, Mortier GR. Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet. 2004 Nov;36(11):1213-8. doi: 10.1038/ng1453. Epub 2004 Oct 17. PMID: 15489854.
- Chatterjee P, Sureka J, Joseph E, Sudhakar S, Chittaranjan S. Intraosseus and extraosseus juxtaarticular calcification: Osteopoikilosis with synovial osteochondromatosis - an association. J Radiol Case Rep. 2009;3(3):1-5. doi: 10.3941/jrcr.v3i3.138. Epub 2009 Mar 1. PMID: 22470645; PMCID: PMC3303297.
- Benli IT, Akalin S, Boysan E, Mumcu EF, Kiş M, Türkoğlu D. Epidemiological, clinical and radiological aspects of osteopoikilosis. J Bone Joint Surg Br. 1992 Jul;74(4):504-6. doi: 10.1302/0301-620X.74B4.1624505. Erratum in: J Bone Joint Surg [Br] 1994 Jul;76(4):683. PMID: 1624505.
- Carpintero P, Abad JA, Serrano P, Serrano JA, Rodríguez P, Castro L. Clinical features of ten cases of osteopoikilosis. Clin Rheumatol. 2004 Dec;23(6):505-8. doi: 10.1007/s10067-004-0935-2. PMID: 15801069.
- Lagier R, Mbakop A, Bigler A. Osteopoikilosis: a radiological and pathological study. Skeletal Radiol. 1984;11(3):161-8. doi: 10.1007/BF00349489. PMID: 6719141.
- Mungovan JA, Tung GA, Lambiase RE, Noto RB, Davis RP. Tc-99m MDP uptake in osteopoikilosis. Clin Nucl Med. 1994 Jan;19(1):6-8. doi: 10.1097/00003072-199401000-00002. PMID: 8137588.
- 10.1016/j.injury.2015.02.005. Epub 2015 Feb 11. PMID: 25707878.
- Woyciechowsky TG, Monticielo MR, Keiserman B, Monticielo OA. Osteopoikilosis: what does the rheumatologist must know about it? Clin Rheumatol. 2012 Apr;31(4):745-8. doi: 10.1007/s10067-011-1916-x. Epub 2012 Jan 14. PMID: 22246417.