More Information
Submitted: January 10, 2023 | Approved: January 23, 2023 | Published: January 24, 2023
How to cite this article: Atallah A, Gabsi S, Hajri M, Hadrich Z, Mestiri H, et al. Non-operative management of perforated jejunal diverticulitis. Arch Case Rep. 2023; 7: 006-007.
DOI: 10.29328/journal.acr.1001066
Copyright License: © 2023 Atallah A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Non-operative management of perforated jejunal diverticulitis
Aziz Atallah, Sofiene Gabsi, Mohamed Hajri, Zied Hadrich* , Hafedh Mestiri and Sahir Omrani
, Hafedh Mestiri and Sahir Omrani
Department of General Surgery, Mongi Slim University Hospital, Faculty of Medicine of Tunis, University of Tunis El Manar, Tunisia
*Address for Correspondence: Zied Hadrich, Department of General Surgery, Mongi Slim University Hospital, Faculty of Medicine of Tunis, University of Tunis El Manar, Tunisia, Email: [email protected]
Diverticula can affect all segments of the gastrointestinal tract, from the esophagus to the colon. In order of decreasing, the jejunoileal location is the least frequent location [1] and has a prevalence of less than 2% of the population [2]. This location was first described by Sommering in 1794 [3]. More than two-thirds of small bowel diverticula occur in the jejunum. They appear mainly after the age of 60 with higher prevalence in males and rarely occur in patients under the age of 40 [4]. Jejunal diverticula are in general multiple and bigger than ileal ones [5]. Most of them are asymptomatic and do not require surgical treatment. Clinical presentations are diverse and not specific with no pathognomonic clinical symptoms.
Because of variable and specific symptoms, diagnosis is most frequently made incidentally or following a complication, causing a delay in treatment. Ten percent of patients with jejunoileal diverticulosis develop complications such as jejunal diverticulitis (the most common complication), perforation, generalized peritonitis, localized abscess, intestinal obstruction, fistula or hemorrhage [6].
Diagnosis is actually made by abdominal Computed Tomography (CT) and management depends on the gravity of the complication and may require surgical treatment in the majority of cases [7].
We describe a case of perforated jejunal diverticula that was successfully managed non-operatively due to an early diagnosis.
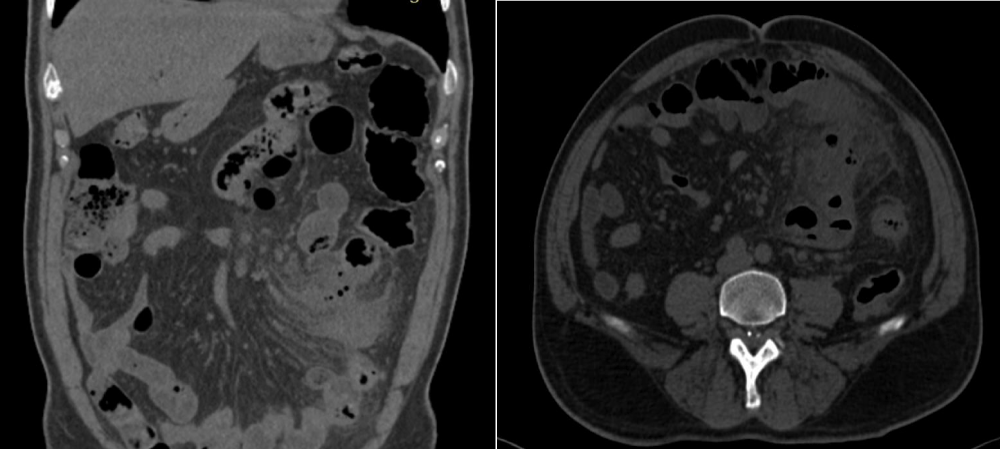
We present a 70 years-old woman, with a background of type 2 diabetes mellitus with no surgical history. She had no relevant family history. She was presented to the emergency department of our hospital with a day of abdominal pain, particularly in the left lower hemi-abdomen. The pain was associated with fever and vomiting. Abdominal examination revealed tenderness of the left lower quadrant. There were no signs of hemodynamic instability. No similar episode was reported in the past. Her blood values were within normal range. Computed tomography of the abdomen was performed which demonstrated densification of the peritoneal fat on the left lower quadrant with a few extra digestive gas bubbles next to a thickened jejunal loop with submucosal edema (Figure 1). There were also multiple uncomplicated left colonic diverticula. Otherwise, there was no ascites and no localized abscess. Given the hemodynamic stability, normal biological tests and the absence of major comorbidities, we opted for non-operative management in this patient associated with strict monitoring. She was managed on the ward with intravenous large-spectrum antibiotics coverage, intravenous hydration with fluids, and bowel rest. The antibiotics of choice in our department were Cefotaxime and Metronidazole. After two days, her vital signs and inflammatory markers remained stable and her pain significantly improved. Her abdomen was completely soft. She was allowed a soft diet. She was discharged on hospital day 4 after the complete disappearance of the pain and resumption of a normal solid diet which was well tolerated. Oral Ciprofloxacin and Metronidazole were continued after leaving the hospital for a 10-day total course of antibiotics. On follow-up after 2 weeks, she had no recurrence of symptoms and clinical examination was strictly normal. After 2 years, she remains well with no other symptoms.
Figure 1: Abdominal Computed Tomography showing a densification of the peritoneal fat on the left lower quadrant with gas bubbles.
Jejunal diverticulosis is a rare condition that occurs after the sixth decade of age. The incidence is higher in men compared to women. Small bowel diverticula tend to be smaller and fewer the more distally one progresses in the gastrointestinal tract. Jejunal location is most common than ileal [8]. Colonic and jejunoileal diverticula can coexist in some patients. A diverticulum can be defined as a saccular structure forming on the outer wall of the affected gastrointestinal tract and formed by one or more of the bowel wall layers. This last point will allow us to differentiate between two different kinds of small bowel diverticula: congenital and acquired diverticula. Congenital diverticula (like Meckel’s diveticulum) contains all the layers of the normal gastrointestinal tract and is located on the antimesenteric border. With this exception, all the ileojejunal diverticula are acquired. This type of diverticula is characterized by herniation of mucosa and submucosa through a defect in the muscular wall, on the mesenteric border at the blood vessel penetration sites. This site of herniation is the weakest area of the bowel wall [9,10]. The etiopathogenesis of acquired jejunoileal diverticula is unclear. The main hypothesis focuses on abnormalities in the smooth muscle or myenteric plexus that can affect the intestinal peristaltisis of the affected small bowel and cause an increased intraluminal pressure [11]. The most common complication of jejunal diverticula is diverticulitis whose incidence ranges from 2% to 6%. It occurs with stasis of the intestinal contents in the diverticulum or secondary to mucosal oedema obstructing the neck of the diverticulum and promoting microbial proliferation within it. Perforation of this diverticulum causes local abscess or severe generalized peritonitis. The clinical presentations are diverse and aspecific: acute abdominal pain, fever, biological infectious syndrom. Abdominal CT is the gold standard for diagnosis which must be established with no delay. Currently, there is no clear concessus on therapeutic strategy of the complicated jejunal diverticulitis. In case of localized abscess with no general signs of sepsis or organ failure, intravenous antibiotics alone or associated with percutaneous drainage combined with strict monitoring can avoid surgery. In the case of serious complications in instable patient with delayed diagnosis, surgical treatment becomes inevitable. In expert hands, laparoscopy can be usefull tool in patient with complicated course after non-operative management.
Jejunal diverticulitis is a rare entity with a specific clinical presentation. Diagnosis is usually made during a complication by abdominal CT. There is no clear consensus on therapeutic strategy. Usually, diagnosis is delayed and its management is surgical. We presented a case of perforated jejunal diverticulitis diagnosed early and successfully managed non-operatively.
- Transue DL, Hanna TN, Shekhani H, Rohatgi S, Khosa F, Johnson JO. Small bowel diverticulitis: an imaging review of an uncommon entity. Emerg Radiol. 2017 Apr;24(2):195-205. doi: 10.1007/s10140-016-1448-4. Epub 2016 Nov 4. PMID: 27815648.
- Kassir R, Boueil-Bourlier A, Baccot S, Abboud K, Dubois J, Petcu CA, Boutet C, Chevalier U, Montveneur M, Cano MI, Ferreira R, Debs T, Tiffet O. Jejuno-ileal diverticulitis: Etiopathogenicity, diagnosis and management. Int J Surg Case Rep. 2015;10:151-3. doi: 10.1016/j.ijscr.2015.03.044. Epub 2015 Mar 26. PMID: 25841158; PMCID: PMC4430128.
- Williams RA, Davidson DD, Serota AI, Wilson SE. Surgical problems of diverticula of the small intestine. Surg Gynecol Obstet. 1981 May;152(5):621-6. PMID: 6784259.
- Giuffrida M, Perrone G, Di Saverio S, Annicchiarico A, Pattonieri V, Bonati E, Tarasconi A, Catena F. Jejunal diverticulitis: Things to know to prevent diagnostic mistake. Acta Biomed. 2021 Apr 30;92(S1):e2021154. doi: 10.23750/abm.v92iS1.9679. PMID: 33944837; PMCID: PMC8142753.
- Sinclair A. Diverticular Disease of the Gastrointestinal Tract. Prim Care. 2017 Dec;44(4):643-654. doi: 10.1016/j.pop.2017.07.007. PMID: 29132526.
- Ojili V, Parizi M, Gunabushanam G. Timely diagnosis of perforated jejunal diverticulitis by computed tomography. J Emerg Med. 2013 Mar;44(3):614-6. doi: 10.1016/j.jemermed.2012.02.046. Epub 2012 May 11. PMID: 22579027.
- Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997 Apr;184(4):383-8. PMID: 9100684.
- Liu CY, Chang WH, Lin SC, Chu CH, Wang TE, Shih SC. Analysis of clinical manifestations of symptomatic acquired jejunoileal diverticular disease. World J Gastroenterol. 2005 Sep 21;11(35):5557-60. doi: 10.3748/wjg.v11.i35.5557. PMID: 16222755; PMCID: PMC4320372.
- Benya EC, Ghahremani GG, Brosnan JJ. Diverticulitis of the jejunum: clinical and radiological features. Gastrointest Radiol. 1991 Winter;16(1):24-8. doi: 10.1007/BF01887297. PMID: 1991603.
- Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007 Apr 21;13(15):2240-2. doi: 10.3748/wjg.v13.i15.2240. PMID: 17465510; PMCID: PMC4146853.
- Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD. Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology. 1983 Sep;85(3):538-47. PMID: 6409704.