More Information
Submitted: January 07, 2023 | Approved: January 17, 2023 | Published: January 18, 2023
How to cite this article: Cheikhrouhou T, Dhaou MB, Hbaieb M, Zitouni H, Mhiri R. Vesicovaginal fistula: an uncommon complication of a perineal burn in a 12-year-old girl. Arch Case Rep. 2023; 7: 001-002.
DOI: 10.29328/journal.acr.1001064
Copyright License: © 2023 Cheikhrouhou T, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Perineal burns; Vesicovaginal fistulas; Girl; Transvaginal approach
Vesicovaginal fistula: an uncommon complication of a perineal burn in a 12-year-old girl
Taycir Cheikhrouhou1,2*, Mahdi Ben Dhaou1,2, Manar Hbaieb1,2, Hayet Zitouni1,2 and Riadh Mhiri1,2
1Department of Pediatric Surgery, Hedi Chaker Hospital, Sfax, Tunisia
2University of Medicine of Sfax, University of Sfax, Sfax, Tunisia
*Address for Correspondence: Taycir Cheikhrouhou, Department of Pediatric Surgery, Hedi Chaker Hospital, University of Medicine of Sfax, University of Sfax, Sfax, Tunisia, Email: [email protected]
Perineal burns are a rare finding in children that may cause severe complications. Vesicovaginal fistulas are an uncommon complication of a perineal burn that can be a tragedy for girls suffering from them. Fistula and/or its treatment are a socially debilitating problem with significant medicolegal implications. We present a rare case of a girl with a history of traumatic perineal burns who was diagnosed with a vesicovaginal fistula and repaired through a transvaginal approach.
Vesicovaginal Fistula (VVF) is an abnormal communication between the bladder and the vagina. It may be located at different levels and occur most of the time in a traumatic context [1]. VVF is rare in girls. They occur most of the time during trauma. This condition has far-reaching social implications on the patients, due to the constant dribbling of urine causing wetting of clothes, the accompanying smell and the constant ostracism, humiliation and destitution [1-4]. The purpose of this observation is to present the case of a thermal burn fistula in a 12-year-old girl and to discuss the management.
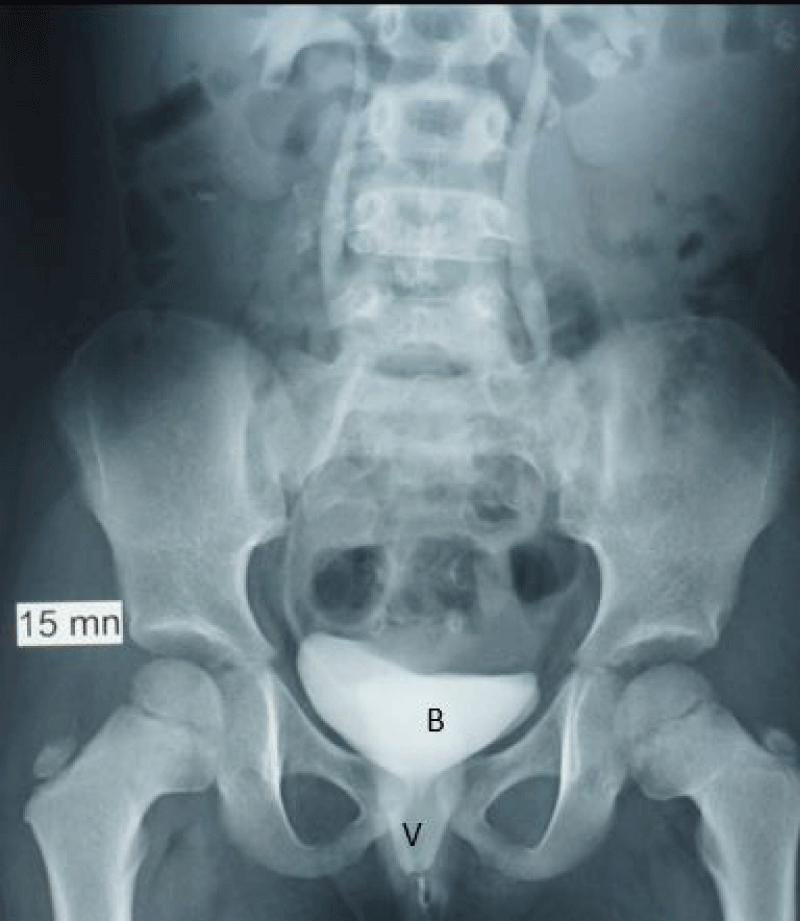
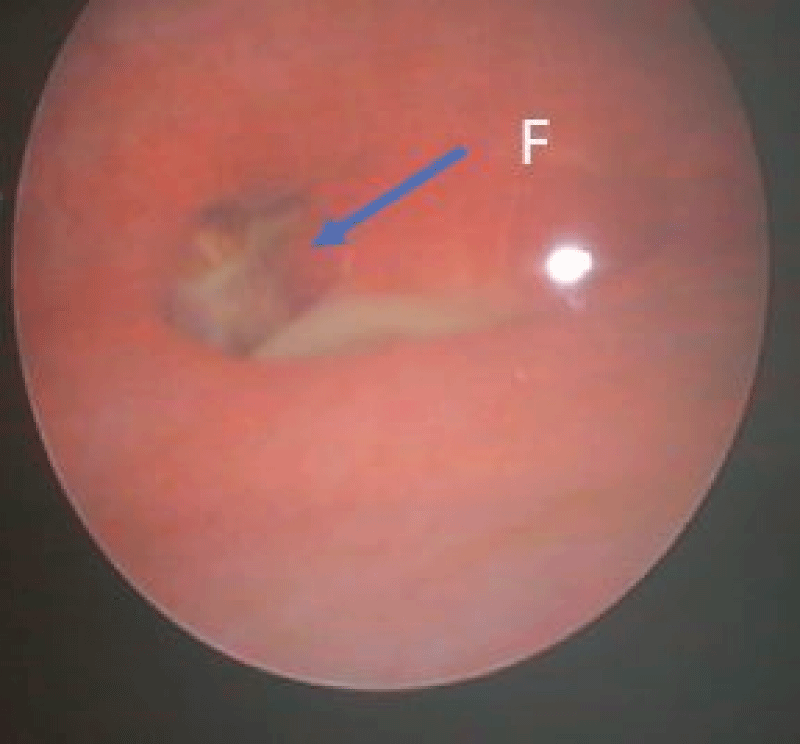
A 12-year-old girl, with a history of thermal burn to 10% of her upper extremities and perineum, was referred to our department approximately 6 months after the traumatic perineal burn, with permanent and involuntary urine loss through the vagina. Physical examination revealed maceration lesions on the external genitalia and the inner face of the thighs. There was a spontaneous and permanent loss of urine through the vagina in orthostatism. At intravenous urography, we noted opacification of the vagina by contrast and urine leakage while standing (Figure 1). At cystoscopy, the diagnosis was established by filling the bladder with a dilute solution of methylene and the fistula is 7 mm in diameter (Figure 2).
Figure 1: Intravenous urography radiography (after 15 minutes) showing the bladder filling and vagina opacification through a vesicovaginal fistula. B: Bladder, V: Vagina.
Figure 2: Endoscopic view showing a 7 mm vesicovaginal fistula. F: Fistula.
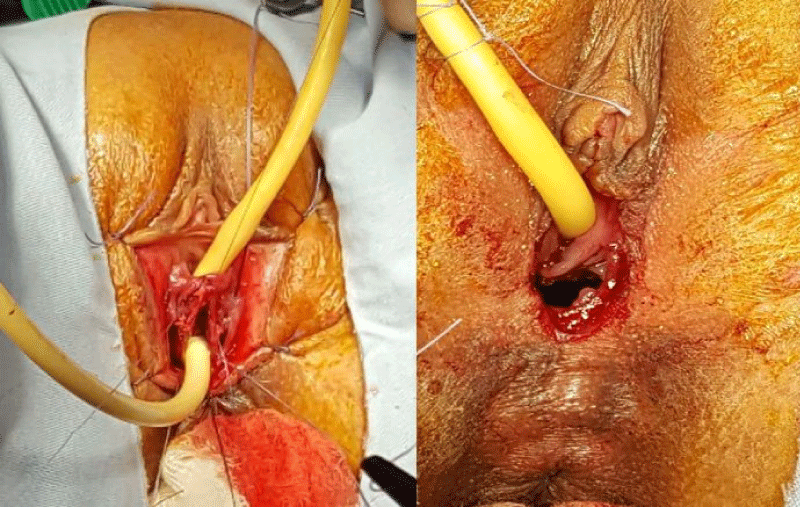
The cure of the fistula was performed through a trans-vaginal approach. We performed an incision around the fistula, followed by a dissection between the vagina and bladder. Each structure was then sutured separately (Figure 3). The postoperative course was uneventful with the satisfactory result with no micturition disorder.
Figure 3: Pre-operative view showing dissection between bladder and vagina.
VVF occurs mostly in obstetric context or is iatrogenic due to surgical procedures in adults [2,3]. In girls, it often occurs in a pelvic trauma context [1]. Involuntary loss of urine in a child first evokes enuresis. When this condition is established, a traumatic etiology is at issue [5,6]. In the case reported, the fistula was the result of a thermal burn of the perineum. Fistula and/or its treatment are serious legal and medical issues. They may have an impact on the quality of sexual life of the patient [7].
VVF identification is usually easy, but a clinical examination in a young girl may be difficult and delicate [2]. We prescribed intravenous urography to seek a possible ureteral injury and appreciate the impact on the upper urinary tract. A detailed assessment of the fistula was done under general anesthesia before performing the surgery. We have also made an intraoperative cystoscopy.
Female vesicourethral lesions are rare and their management remains a challenge. Little is known about the surgical techniques used to treat fistula in children. It is therefore logical to refer to techniques used in adult to manage this condition [1–4]. Key points are the excision of the fistula edge and the separate closure of each layer. VVF management difficulties are linked to the risk of urinary incontinence following rehabilitation due to sphincter damage [2]. The choice of surgical approach depends on the familiarity of the approach by the surgeon, the location of the fistula, available space in the vaginal cavity, the need for ancillary procedures such as ureteric reimplantation and the feasibility of obtaining necessary interposition flaps [8].
The transvaginal route for repair is preferred as it has low morbidity, higher success rates and minimal complications. Younger age and a smaller fistula size were significantly associated with successful anatomical closure [7]. In our case, the cure of the fistula was performed through a transvaginal approach. An incision around the fistula followed by dissection between the vagina and bladder. This allowed us to cure the fistula with a satisfactory postoperative result with no micturition disorder due to sphincter damage.
VVF following perineal burns in girls has a direct bearing on the quality of life with physical, functional, sexual and psychological ramifications. Prompt diagnosis and timely repair are essential for the successful management of these cases. Medico-legal aspects should be always taken into account.
Consent for publication: The parents of the patient have consented to the use of clinical photographs for publication and the research process.
- Ahmed S, Neel KF. Urethral injury in girls with fractured pelvis following blunt abdominal trauma. Br J Urol. 1996 Sep;78(3):450-3. doi: 10.1046/j.1464-410x.1996.00096.x. PMID: 8881960.
- Pushkar DY, Dyakov VV, Kosko JW, Kasyan GR. Management of urethrovaginal fistulas. Eur Urol. 2006 Nov;50(5):1000-5. doi: 10.1016/j.eururo.2006.08.002. Epub 2006 Aug 15. PMID: 16945476.
- Ockrim JL, Greenwell TJ, Foley CL, Wood DN, Shah PJ. A tertiary experience of vesico-vaginal and urethro-vaginal fistula repair: factors predicting success. BJU Int. 2009 Apr;103(8):1122-6. doi: 10.1111/j.1464-410X.2008.08237.x. Epub 2009 Jan 20. PMID: 19154500.
- Coulibaly N, Sangaré IS. Urethrovaginal fistula in a 5-year-old girl. Case Rep Urol. 2015;2015:202059. doi: 10.1155/2015/202059. Epub 2015 Apr 12. PMID: 25954566; PMCID: PMC4410752.
- Venn SN, Greenwell TJ, Mundy AR. Pelvic fracture injuries of the female urethra. BJU Int. 1999 Apr;83(6):626-30. doi: 10.1046/j.1464-410x.1999.00001.x. PMID: 10233569.
- Atan A, Tuncel A, Aslan Y. Treatment of refractory urethrovaginal fistula using rectus abdominis muscle flap in a six-year-old girl. Urology. 2007 Feb;69(2):384.e11-3. doi: 10.1016/j.urology.2006.11.023. PMID: 17320687.
- Kapoor R, Ansari MS, Singh P, Gupta P, Khurana N, Mandhani A, Dubey D, Srivastava A, Kumar A. Management of vesicovaginal fistula: An experience of 52 cases with a rationalized algorithm for choosing the transvaginal or transabdominal approach. Indian J Urol. 2007 Oct;23(4):372-6. doi: 10.4103/0970-1591.36709. PMID: 19718291; PMCID: PMC2721567.
- Rajaian S, Pragatheeswarane M, Panda A. Vesicovaginal fistula: Review and recent trends. Indian J Urol. 2019 Oct-Dec;35(4):250-258. doi: 10.4103/iju.IJU_147_19. PMID: 31619862; PMCID: PMC6792412.