More Information
Submitted: November 07, 2022 | Approved: November 17, 2022 | Published: November 18, 2022
How to cite this article: Reinhold M, Bonacker J, Driesen T, Lehmann W. Neglected percutaneous rod extrusion following posterior occipitocervical instrumentation: a case report. Arch Case Rep. 2022; 6: 024-026.
DOI: 10.29328/journal.acr.1001063
Copyright License: © 2022 Reinhold M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Percutaneous implement extrusion; Implant failure; Complication; Spinal surgery occipitocervical junction
Neglected percutaneous rod extrusion following posterior occipitocervical instrumentation: a case report
Maximilian Reinhold1*, Johannes Bonacker2, Tobias Driesen1 and Wolfgang Lehmann1
1Department of Trauma, Orthopaedic and Plastic Surgery, University Medical Center
Goettingen, Robert-Koch-Str. 40, 37099 Goettingen, Germany
2Department of Traumatology, Orthopaedics and Hand Surgery, Klinikum Suedstadt
Rostock, Südring 81, 18059 Rostock, Germany
*Address for Correspondence: Dr. Maximilian Reinhold, MBA, MD, Department of Trauma, Orthopaedic and Plastic Surgery, University Medical Center Goettingen, Robert-Koch-Str. 40, 37099 Goettingen, Germany, Email: [email protected]
Purpose: The extrusion of implant material is a rare complication but has been reported in several cases following anterior cervical spine surgery. A posterior spontaneous percutaneous rod extrusion after rigid occipitocervical (OC) instrumentation (screw and rod construct) has not been reported yet. The authors discuss potential complications after cervical spine surgery and its clinical management.
Methods: This is a case report of a 56-year-old patient after posterior OC spine surgery with initially unobserved implant failure and posterior percutaneous rod extrusion. The implant failure with a missing rod has been documented 4 years later during a routine follow-up visit.
Results: At the four-year follow-up, the asymptomatic patient presented with a stable occipitocervical junction and an improved range of motion after generalized sepsis with an epidural spinal abscess, decompression and posterior OC instrumentation. A computed tomography scan of the implant failure of a broken rod was noticed two years postoperatively. The patient failed to return to the clinic. For years postoperatively he returned to the clinic and the broken rod could not be detectable in-situ on the X-rays anymore.
Conclusion: The posterior percutaneous rod extrusion following an OC instrumentation not noticed by the patient, is a very rare complication that has not been described in the literature yet. Once seen back in the clinic, the patient unexpectedly reported an improved ROM without neck pain. Usually, revision surgery or implant removal is recommended if an implant failure is documented.
The local anatomy of the occipitocervical junction is complex and consists of the occiput, first and second vertebra near relevant, vital neurovascular structures. The treatment of unstable disorders of the craniovertebral region, e.g. fractures, spinal abscesses, or other degenerative conditions, is challenging and sometimes different to treat, especially in an emergent situation [1]. Sepsis and spondylodiscitis can evolve into a life-threatening, unstable situation that renders immediate decompression and instrumentation to restore the stability and prevention of neurologic deficits that at this level of the cervical spine can an instant breathing arrest and eventually death. A good treatment plan is needed that should follow established algorithms for spondylodiscitis similar to those available for the thoracic and lumbar spine [2].
Different potentially life-threatening complications after cervical and occipitocervical spinal fusions have been described [3,4]. Implant failure and metal extrusions out of the patient’s body are rare complications. To the knowledge of the authors, this has only been described in some case reports following anterior fusion surgery of the cervical spine [5]. This case report is the first description of a percutaneous (“disappeared”) rod and metal extrusion of a patient having had after posterior instrumentation of the craniovertebral junction. The surgical intervention was indicated as an emergent decompression of an epidural spinal abscess with cord compression.
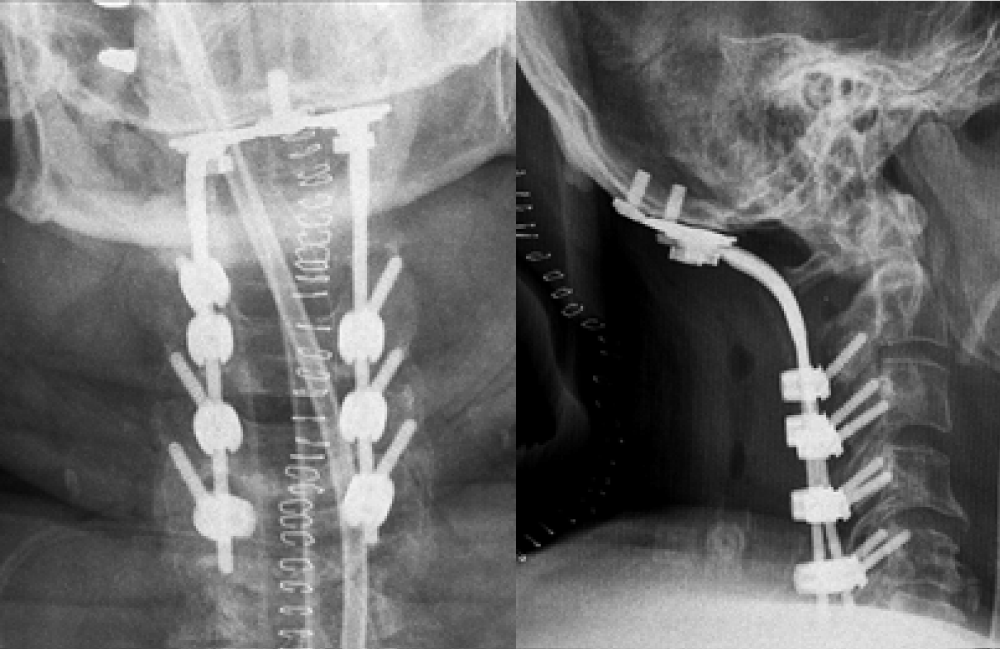
A 56-years old patient was admitted to the hospital with necrotizing fasciitis at both forearms after he received infusion therapy in an outpatient clinic. He developed a generalized septic condition and underwent multiple emergent orthopedic surgeries in order to control the infections. This included repeated soft tissue debridements and amputation of the left lower extremity. Additionally, as a consequence of the fulminant sepsis with streptococcus spp. he developed an epidural abscess at the occipitocervical junction, too. Due to an ongoing clinically symptomatic spinal cord compression with myelopathy an emergency posterior decompression of the neural elements, abscess drainage and instrumentation from the occiput (C0) to the fifth cervical vertebra (C5) was necessary. The necessary stability was restored with an occipital plate, screw and bilateral rod construct (Figure 1). Eventually the patient survived and was discharged after a long hospital stay and several months of rehabilitation.
Figure 1: Early postoperative a.p. and lateral films following posterior occipito-cervical instrumation (C0-C5).
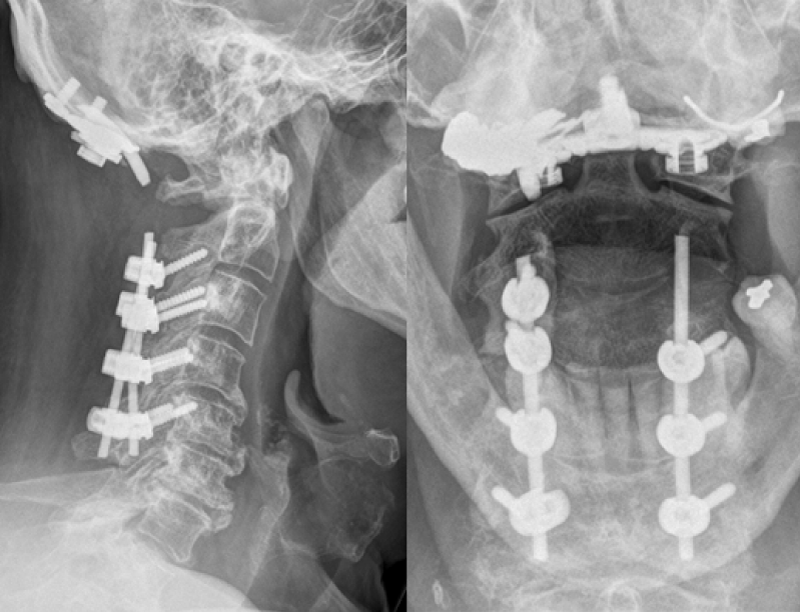
Two years later, the patient returned to the clinic for a follow-up visit. A bilateral implant failure with bilateral broken rods at the C1/2 level was seen in the corresponding X-rays (Figure 2). The patient did not report any cervical spine trauma, pain, or other complaints, despite he could move his head much better again with a quite satisfactory improved range of motion, mild discomfort and tolerable neck pain compared to the situation right after surgery. Revision surgery for partial implant removal and re-instrumentation of the broken rods was recommended to the patient. The patient failed to return to the clinic as recommended.
Figure 2: X-Ray ap 4-year follow-up with missing left-sided rod.
It was not until four years later, that the patient returned to the clinic again and could be seen next. Once questioned about his well-being or if he had noticed anything unusual, he reported approximately six months before one morning he had noticed something that to him looked like a “small metal wire” on his pillow. Despite he didn’t know where it was from other than he was treated by his family physician for “furuncle in the neck” at this time, he had not paid particular attention to it, since the furuncle disappeared shortly afterward. In the meantime, he had discharged that strange “piece of metal” in his bed and thrown it away.
However, at this point in time radiographs of the cervical spine showed a missing rod. In conclusion given the medical history and temporary “furuncle in the neck”, that was successfully treated by the family physician with local antiseptics, it must have been the rod and missing part of instrumentation that extruded the musculature, soft tissues, and skin, which had otherwise healed uneventfully.
Still, there were no signs of instability or complaints with a good range of motion. Once informed about the situation and options, the patient decided against further surgery.
Surgical techniques and spinal instrumentations are well-established for a variety of pathologies at the occipitocervical junction. Traumatic fractures, fracture subluxation, neoplastic or metastatic spinal diseases [6] and infections with lytic lesions oftentimes can be stabilized best with posterior instrumentation, e.g. plate, screw, and rod constructs that offer favorable biomechanical and clinical outcomes [7].
Given the complex anatomy of the upper cervical spine including the occiput, a thorough preoperative plan for the individual patient’s situation is mandatory to avoid potential complications related to neurovascular injuries or implant failure [2].
Leckie, et al. [8] in a retrospective study investigated the spectrum of perioperative complications in cervical spine surgery. This includes implant failure (broken rods or screws) or loosening (screw pull-out or cut-out) in case of a pseudarthrosis or failed spinal fusion as it was only the instrumentation (no bone transplant or fused joints) that provided enough stability to heal the abscess and keep control of the local infection.
Complication rates are highest in patients with posterior or combined anterior-posterior surgery. Complication rates and adverse events most significantly occur in multi-level posterior or revision surgeries in elderly patients [8].
Implant failure has been reported following anterior and/or posterior surgery. In a clinical study, twenty-seven patients with craniocervical instability underwent OC fusion with a screw-rod system and eight patients had an implant-related failure (29.6%) after a mean follow-up time of 7.2 years. The authors conclude that stronger rods may prevent implant failure and broken rods [9]. In a systematic review of OC fusion techniques, Winegar, et al. [7] reported an implant (screw/rod) failure rate of 7.9%. In a retrospective study by He, et al. [10] within the subgroup of patients with OC spinal fusion and instrumentation (n = 262), four (1.6%) patients had an implant failure. In a retrospective study, Shamij, et al. [4] observed the highest complication rates in posterior surgeries for multilevel fusion.
Implant extrusion from the body can occur after implant loosening and dislodgement. It is a rare, but severe complication that may also become a life-threatening situation. In such cases, an interdisciplinary treatment strategy has been recommended [11]. The migration of implants after anterior cervical plates through the esophago-pharyngeal wall can cause dysphagia and postoperative infections. This has been described in several studies and case reports [3,12,13] Klicken oder tippen Sie hier, um Text einzugeben... Dysphagia and mechanical irritation caused by loosened, displaced implants oftentimes require complex revision surgeries [14].
To the knowledge of the authors, this is the first case of implant failure with a delayed spontaneous percutaneous partial rod extrusion ex-vivo following posterior occipito-cervical instrumentation. Notably, the situation was misinterpreted and treated as a skin infection and had healed uneventfully once the implant had made its way backward through the muscular and soft tissues of the neck at the C1/2 level. Nevertheless, the authors do not recommend neglect of broken implants, especially in cases of persistent spinal instability that can usually only be treated once permanent and solid bony fusion (spondylodesis) is achieved. Otherwise, revision surgery is strongly recommended to avoid implant-related postoperative complications [11].
The limitation of this study is that this is a single case of unique complication in a patient with a limited understanding of his medical condition and compliance. As a consequence, patients once again should be advised and informed to pay particular attention to the surgical site and have a low threshold to ask and return to the clinic, if they observe or feel anything unusual.
Posterior occipitocervical instrumentation and fusion techniques are well-established surgical procedures to address different neoplastic, infectious and posttraumatic pathologies with spinal instability. This is the first case report of a neglected implant failure with a delayed percutaneous partial rod extrusion following posterior occipitocervical instrumentation that had otherwise healed uneventfully. Once informed and educated about the options, the patient decided against revision surgery given the good clinical outcome with improved range of motion at follow-up.
- Kukreja S, Ambekar S, Ahmed OI, Menger RP, Sin AH, Nanda A. Impact of elective versus emergent admission on perioperative complications and resource utilization in lumbar fusion. Clin Neurol Neurosurg. 2015 Sep;136:52-60. doi: 10.1016/j.clineuro.2015.05.015. Epub 2015 May 22. PMID: 26067722.
- Pitzen T, Meinig H, Drumm J. Challenges and characteristics of spondylodiscitis of the cervical spine. Der Orthopade. 2012; 41:759-63. https://doi.org/10.1007/s00132-012-1919-6
- Geyer TE, Foy MA. Oral extrusion of a screw after anterior cervical spine plating. Spine (Phila Pa 1976). 2001 Aug 15;26(16):1814-6. doi: 10.1097/00007632-200108150-00019. PMID: 11493857.
- Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009 Jan-Feb;9(1):31-8. doi: 10.1016/j.spinee.2008.07.005. Epub 2008 Sep 14. PMID: 18790678.
- Geyer TE, Foy MA. Oral extrusion of a screw after anterior cervical spine plating. Spine (Phila Pa 1976). 2001 Aug 15;26(16):1814-6. doi: 10.1097/00007632-200108150-00019. PMID: 11493857.
- Sapkas G, Papadakis SA, Segkos D, Kateros K, Tsakotos G, Katonis P. Posterior instrumentation for occipitocervical fusion. Open Orthop J. 2011;5:209-18. doi: 10.2174/1874325001105010209. Epub 2011 Jun 2. PMID: 21772931; PMCID: PMC3139273.
- Winegar CD, Lawrence JP, Friel BC, Fernandez C, Hong J, Maltenfort M, Anderson PA, Vaccaro AR. A systematic review of occipital cervical fusion: techniques and outcomes. J Neurosurg Spine. 2010 Jul;13(1):5-16. doi: 10.3171/2010.3.SPINE08143. PMID: 20594011.
- Leckie S, Yoon ST, Isaacs R, Radcliff K, Fessler R, Haid R Jr, Traynelis V. Perioperative Complications of Cervical Spine Surgery: Analysis of a Prospectively Gathered Database through the Association for Collaborative Spinal Research. Global Spine J. 2016 Nov;6(7):640-649. doi: 10.1055/s-0035-1570089. Epub 2015 Dec 15. PMID: 27781183; PMCID: PMC5077719.
- Ando M, Tamaki T, Yoshida M, Sasaki S, Toge Y, et al. Surgical site infection in spinal surgery: a comparative study between 2-octyl-cyanoacrylate and staples for wound closure. Eur Spine J. 2014 Apr;23(4):854-62. doi: 10.1007/s00586-014-3202-5. Epub 2014 Feb 1. PMID: 24487558; PMCID: PMC3960412.
- He B, Yan L, Xu Z, Chang Z, Hao D. The causes and treatment strategies for the postoperative complications of occipitocervical fusion: a 316 cases retrospective analysis. Eur Spine J. 2014 Aug;23(8):1720-4. doi: 10.1007/s00586-014-3354-3. Epub 2014 May 18. PMID: 24838504.
- Tang C, Li GZ, Kang M, Liao YH, Tang Q, Zhong J. Revision surgery after rod breakage in a patient with occipitocervical fusion: A case report. Medicine (Baltimore). 2018 Apr;97(15):e0441. doi: 10.1097/MD.0000000000010441. PMID: 29642217; PMCID: PMC5908617.
- Salis G, Pittore B, Balata G, Bozzo C. A rare case of hypopharyngeal screw migration after spine stabilization with plating. Case Rep Otolaryngol. 2013;2013:475285. doi: 10.1155/2013/475285. Epub 2013 Jun 9. PMID: 23841003; PMCID: PMC3690641.
- Smith GA, Pace J, Corriveau M, Lee S, Mroz TE, et al. Incidence and Outcomes of Acute Implant Extrusion Following Anterior Cervical Spine Surgery. Global Spine J. 2017 Apr;7(1 Suppl):40S-45S. doi: 10.1177/2192568216686752. Epub 2017 Apr 1. PMID: 28451490; PMCID: PMC5400179.
- Hong J, Lim S. Dysphagia after Occipitocervical Fusion. N Engl J Med. 2017 Jun 1;376(22):e46. doi: 10.1056/NEJMicm1610752. PMID: 28564573.