More Information
Submitted: October 31, 2019 | Approved: January 11, 2021 | Published: January 12, 2021
How to cite this article: Corrêa S. PET/MRI, aiming to improve the target for Fractionated Stereotactic Radiotherapy (FSRT) in recurrence of resected skull base meningioma after 2 years: Case report. Arch Case Rep. 2021; 5: 001-003.
DOI: 10.29328/journal.acr.1001044
Copyright License: © 2021 Corrêa S. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Meningioma; PET/MRI; Radiotherapy planning; Target definition
PET/MRI, aiming to improve the target for Fractionated Stereotactic Radiotherapy (FSRT) in recurrence of resected skull base meningioma after 2 years: Case report
Sebastião Corrêa*
Radiation Oncology Department, Hospital Sírio-Libanês, Rua Dona Adma Jafet, 91 - Bela Vista, CEP 01308-050 Sao Paulo, SP, Brazil
*Address for Correspondence: Sebastião Corrêa, Radiation Oncology Department, Hospital Sírio-Libanês, Rua Dona Adma Jafet, 91 - Bela Vista, CEP 01308-050 Sao Paulo, SP, Brazil, Email: [email protected]
The increasing use of highly conformal radiation deliberates a higher accurate targeting. Contouring and clinical judgment are presumably the crucial point, thus positron emission tomography/magnetic resonance imaging PET/MRI with somatostatin analogs appears to be useful in radiotherapy target definition. A case report of a 43-year-old woman presented with a recurrence of a meningioma (World Health Organization group I classification) in skull base, 2 years after resection. Magnetic resonance imaging (MRI) revealed a left sided skull base mass on sphenoid wing, anterior clinoid and with a soft tissue component in the lateral portion of the orbit.
Contrast-enhanced MRI and a computed tomography (CT) dedicated were used to the radiotherapy planning. Aiming an improvement on target volume delineation, 68Ga-DOTATOC-PET/MRI was also performed due the difficult localization of the tumor in skull base. Was treated using intensity-modulated radiotherapy (IMRT) to a total dose of 54 Gy in 28 fractions. It was prescribed to the planning target volume (PTV), defined based of both imaging modalities. In our case PET/MRI helped to define the target, which volume becomes bigger than that based exclusively on MRI and CT.
Meningiomas are tumours derived from meningothelial cells. They represent one of the largest groups of primary intracranial tumors. In about 80%, they are slow growing, of a benign histology, and have a higher prevalence in women than in men (2:1). However, especially high-grade meningiomas are known for their rapid growth and a significantly increased likelihood of recurrence after treatment. According to the WHO classification of tumors of the central nervous system, meningiomas can be classified into three grades: I – benign meningiomas, II – atypical meningiomas, and III – anaplastic/malignant meningiomas. Most meningiomas are grade I (90%); grade II represents 5% – 7% of all meningiomas and grade III constitutes 1% – 3%. The treatment of meningiomas can be challenging due their proximity to organs like the brainstem or cranial nerves.
Surgery remains the treatment of choice, reaching long-term control rates after complete tumor removal in low-grade meningiomas. Radiation therapy (RT) has become of great importance as a primary or adjuvant treatment option; especially for patients suffering from high-grade meningiomas, subtotal resection, or poor physical condition. Until now, RT treatment planning has been based mainly on computed tomography and contrast-enhanced magnetic resonance imaging. However, in the case of quasi-planar growth, these imaging techniques have limitations concerning the visualization of the exact tumor extension. Thus, positron emission tomography (PET) combined with MRI (PET/MRI) is highly valuable as an additional imaging modality for more accurate target volume delineation. Meningiomas are known to express somatostatin receptor subtype 2. Thus, the gallium-68-labeled somatostatin-receptor ligand 1,4,7,10 - tetraazacyclododecane - 1,4,7,10 - tetraacetic acid (DOTA) - D-Phe1 - Tyr3 -octreotide (TOC) (68Ga-DOTATOC), can be used as a biomarker to visualize the extension of meningiomas with PET.
This combined imaging technique allows the acquisition of images from two modalities, PET and MRI, within a single examination without moving the patient between modes. Possibility of multiparametric imaging in addition to simultaneous acquisition of molecular processes and high-resolution morphology offers a variety of perspectives for human brain imaging. Our purpose was to explore the target volume delineation based on simultaneous 68Ga-DOTATOC-PET/MRI in comparison to that on MRI with intensity-modulated radiotherapy (IMRT) for treatment of a skull base meningioma.
A 43-year-old woman presented with a recurrence of a meningioma (World Health Organization group I classification) in skull base, 2 years after resection. The meningioma was a mass into the left sphenoid wing and anterior clinoid. There was a soft tissue component in the lateral portion of the left orbit, extends near to the orbital apex in contact with optic nerve and lateral rectus muscle.
The patient experienced clinical symptoms, most in left side with diplopia, visual cloudiness, visual proptosis and headache; consisting of a recurrence on MR imaging.
Was prescribed a treatment by an experienced interdisciplinary tumor board. She was examined with a MRI and CT dedicated to planning. To improve the target volume delineation purposes a PET/MRI were requested due the difficult localization of the tumor.
In terms of IMRT treatment, a total dose of 54 Gy in 28 fractions, 5 days a week. It was prescribed to the planning target volume (PTV), defined on the basis of MRI and 68Ga-DOTATOC-PET/MRI imaging. For accurate patient positioning, a thermoplastic mask system was used in addition to onboard position verification with daily image-guidance (IGRT) by cone beam CT system.
PET/MRI imaging
Metabolic images obtained in PET/MRI hybrid equipment associated to multiplanar acquisitions of T2 - weighted images, FLAIR, diffuse, magnetic susceptibility and T1 before and after venous injection of paramagnetic contrast.
Signs of left fronto-orbitary craniotomy with local magnetic susceptibility artifacts, also related to the osteosynthesis material that lines the orbital ceiling on this side. It presents thickening and meningeal enhancement in the left frontal convexity and underlying craniotomy, which extends along the major and minor wings of the sphenoid, to the left cavernous sinus, involving the cavernous segment of the internal carotid artery (which remains patent and preserved caliber). It extends through the proximal maxillary and mandibular divisions of the left trigeminal nerve, and also the lateral wall of the left orbit, in intimate contact with the lateral and superior straight muscles, invading superolateral intraconal fat, occupying part of the orbital apice, where it compresses the optic nerve (which seems to maintain its usual signal in FLAIR). There was a sharp increase in the concentration of the somatostatin analogue in areas of heterogeneous thickening and enhancement of the major and minor wings of the left sphenoid, with extension to the soft parts in the lateral portion of the orbit, maintaining broad contact with the lateral rectus muscle (SUV max: 42,7).
The areas of meningeo thickening in the anterior fossa, at the ceiling of the orbit and in the front temporal region on the left also present a higher concentration of radiopharmaceutical (SUV max: 21, 6).
Target volume delineation for IMRT
Target volume delineation plays a crucial role in the planning of high precision radiation therapy preserving to the maximum the organs at risk (OAR) in critical locations. In meningiomas, the gross tumor volume (GTV) and clinical target volume (CTV) are delineated based on image fusion of contrast-enhanced CT and MRI.
However, in some cases, in tumors located at the skull base, it is difficult to differentiate between normal and tumor tissue. Furthermore, in postoperative MRI with inconclusive findings, PET may aid in the identification of active tumor remnants in the planning of adjuvant RT after subtotal or partial tumor resection. In these cases, PET imaging may add helpful information. For RT planning, it is necessary to fuse PET/MRI with the simulation CT. Thus in radiation treatment it could significantly influence GTV delineation.
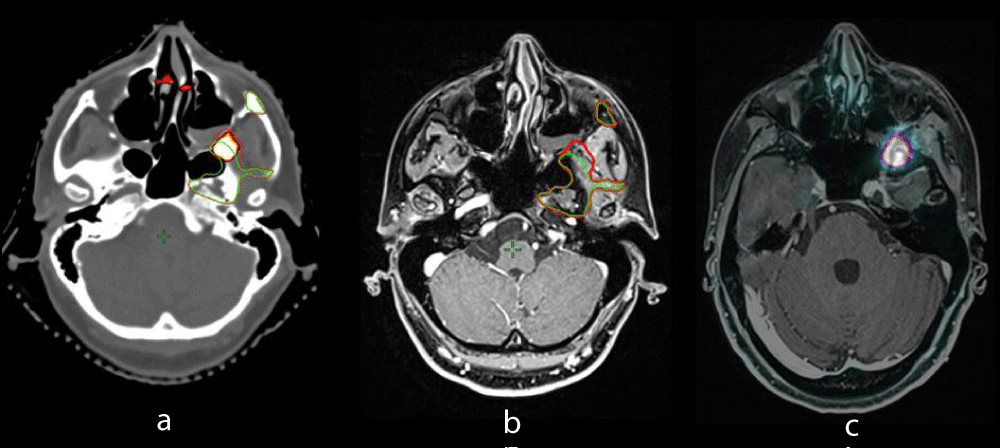
The most different sites of contouring were bone and the post-operative bed. The PET/MRI image bring a larger volume in left sphenoid, with extension to the soft parts in the lateral of orbit and in the superior GTV’s limits on temporal bone. Therefore we found a difference higher than 5% on the respective target volumes (Figure 1).
Figure 1: Regions of interest contoured on PET/MRI and MR images vs. MR images. (1a) Green outline = GTV_MRI; red outline = GTV_PET/MRI. (1b) Green outline = GTV_MRI; red outline = GTV_PET/MRI. (1c) Red outline = GTV_PET/MRI showing areas out the PTV even with MR.
The use of 68Ga-DOTATOC-PET/MRI may be a useful and promising tool on delineating meningiomas. It appears to improve accurate showing areas out of PTV and also to corroborate to spare organs at risk (OARs).
As well the PET/RM might reduce interobserver variability on contouring. Whereas the control rates are about 80% after radiotherapy in 10 years, the lack of consistency in contouring could be inquired. However, these data are obtained from series using older treatment methods where tissue adjacent to the target inevitably received therapeutic radiation doses, thereby reducing the effect of variation in target definition on disease control.
Sharper dose gradients achievable with IMRT and radiosurgery necessitate greater confidence in target delineation to maintain the high rates of local control. Indeed other authors have shown that the integration of additional imaging modalities does not necessarily reduce the inter-observer variability (IOV) in contouring and could even compound uncertainties. We envisage that the routine indications for PET use in radiotherapy planning will increase once sensitivity is better defined as it could then be used to minimize target volumes, particularly adjacent to OARs, where ‘erring on the side of caution’ is undesirable.
However, currently we feel that routine 68Ga- DOTATATE PET imaging for meningioma radiotherapy planning is not warranted. It may still be useful for clinicians who contour very tight volumes and could add additional information in select cases where tumor boundaries on MRI and CT are unclear. Our findings indicate PET may be most helpful for meningiomas in the skull base, and if a larger study was to be carried out, it may be prudent to restrict inclusion to meningiomas in that region.
The use of simultaneous PET/MR imaging is clinically feasible and benefits for accurate target volume delineation, mainly for cases of meningioma in skull base, with highly conformal RT techniques. Our experience showed that there a more detailed visualization especially on bones and in infiltrative regions after surgery. Therefore we concluded due the high sensitivity and specificity of 68Ga-DOTATOCPET jointly with the morphological visualization on MRI might become the pattern imaging method. Nevertheless, no broad conclusions can be drawn as only a case reported, and forthcoming researches aiming to evaluate the real clinical benefit.