Case Report
Gastric Mucosal Calcinosis
Vedat Goral1*, Irem Ozover2 and Ilknur Turkmen2
1Medipol University Medical Faculty Gastroenterology Department, Istanbul, Turkey
2Medipol University Medical Faculty Pathology Department, Ista, Turkey
*Address for Correspondence: Vedat Goral, Medipol University Medical Faculty Gastroenterology Department, Istanbul, Turkey, Email: [email protected]
Dates: Submitted: 21 September 2017; Approved: 26 September 2017; Published: 27 September 2017
How to cite this article: Goral V, Ozover I, Turkmen I. Gastric Mucosal Calcinosis. Arch Case Rep. 2017; 1: 003-005. DOI: 10.29328/journal.hjcr.1001002
Copyright License: © 2017 Goral V, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Gastric mucosal calcinosis
Abstract
Gastric mucosal calcinosis is a very rare pathology of the gastric mucosa. It may develop secondary to several diseases but may also be idiopathic in some cases. In this case, gastric mucosal calcinosis was diagnosed with endoscopic biopsy performed for a patient who presented to our clinic with heartburn and abdominal discomfort. This case involves a very rare gastric pathology, and is being studied here with reference to literature data.
Case Report
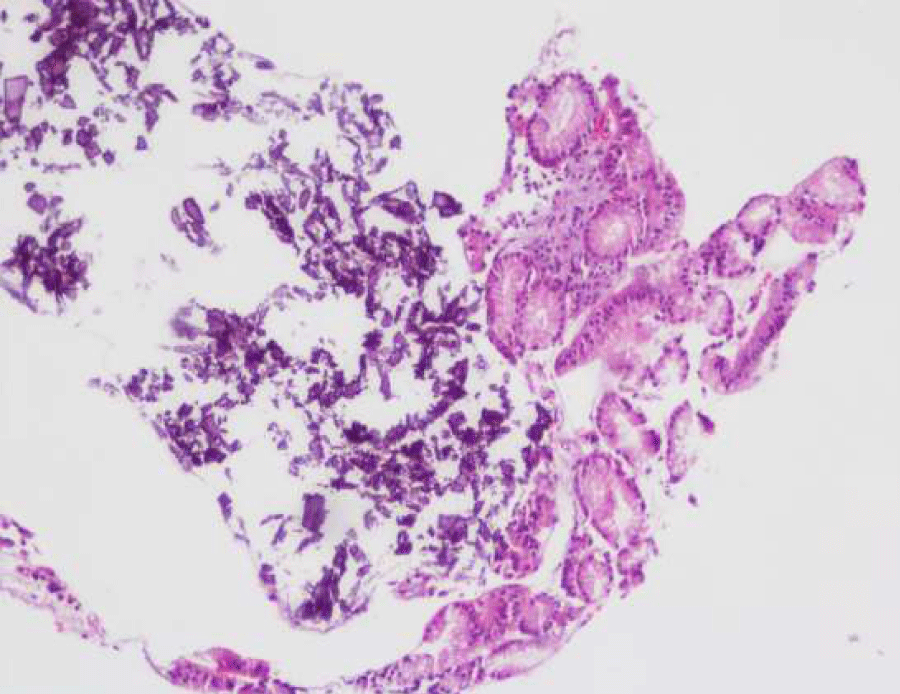
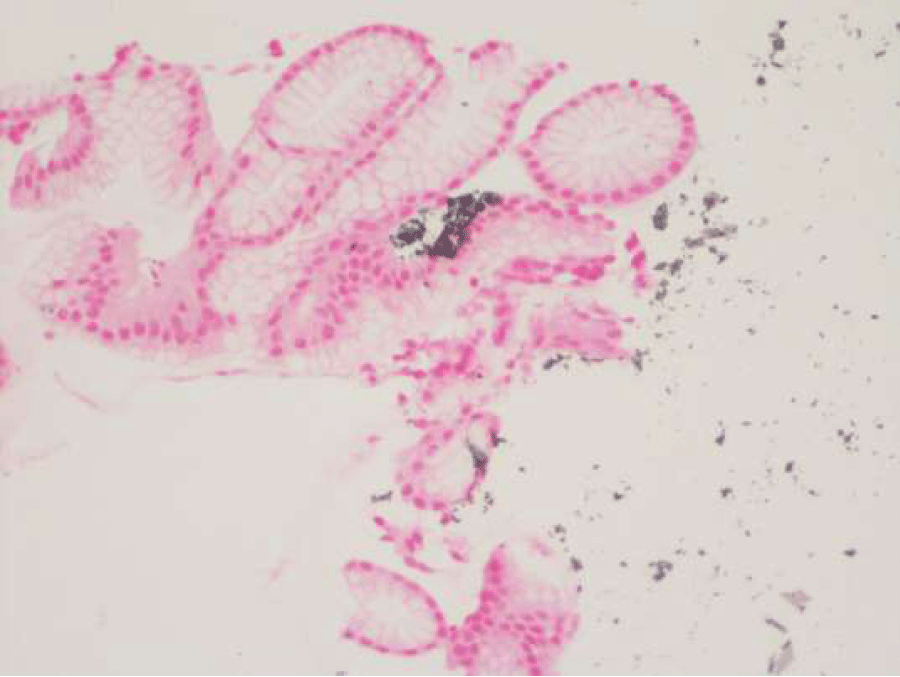
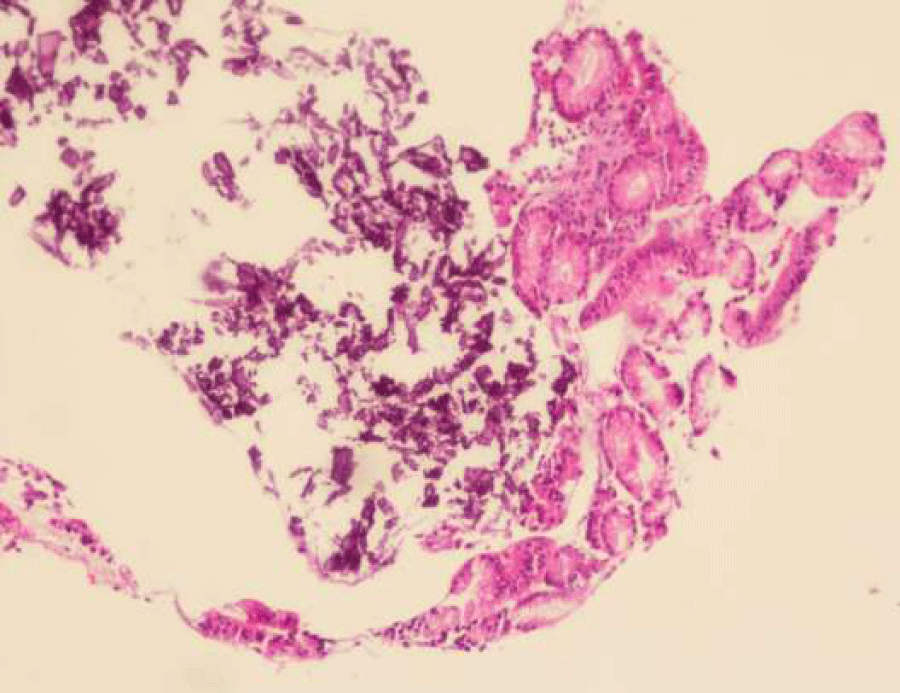
The endoscopy performed for the 43-years-old male patient who presented to our clinic with dyspeptic and epigastric pain demonstrated Mallory-Weiss syndrome and chronic gastritis. No white, flat plaques were seen with endoscopy. The result of the biopsy with haematoxylin and eosin (H&E) staining performed on the material taken during endoscopy was reported as chronic gastritis and gastric mucosal calcinosis characterized by chronic infiltrate. Helicobacter pylori was negative and no atrophy, intestinal metaplasia or dysplasia was detected. Staining with Von Cossa clearly demonstrated gastric mucosal calcinosis with large, dense, irregular C accumulation (Figure 1A, 1B, 2A, 2B). Pathology department’s opinion was that the mucosal calcinosis observed in the corpus mucosa could be associated with calcium dysregulation and could also be secondary to medication, and recommended analyzing correlation with clinical findings. Patient’s physical examination and routine hematology yielded results that were within normal ranges. USG revealed hepatosteatosis. Abdominal computed tomography (CT) also yielded normal results. Serum PTH was 31.96 pg/ml [N: 15-65 pg/ml], serum calcium was 10.69 mg/dl [N: 8.6-10 mg/dl] and serum phosphorus was 4.88 mg/dl [N: 2.6-4.5 mg/dl]. The opinion of endocrinology was therefore sought. Endocrinology department docor’s said that there is no hyperparathyroidism. Therefore, hyperparathyroidism was not reported. It was considered to be due to the antacids the patient was taking. The patient was given empiric 40 mg pantoprazole to be taken in the morning before breakfast on empty stomach and 20 ng famotidine to be taken at bedtime. When the patient returned for follow-up, he was free of gastric complaints. Gastric mucosal calcinosis is a very rare pathologic diagnosis and we aimed to present this case with reference to the literature data.
Figure 1A: Amorphous basophilic calcium deposits in gastric mucosa (A, HE, x100) verified with Voncossa stain (B, Von Cossa, x200).
Figure 1B: Von Cossa x 20 Amorphous basophilic calcium deposits in gastric mucosa (A, HE, x100) verified with Voncossa stain (B, Von Cossa, x200).
Figure 2A: Von Cossa x 20 Amorphous basophilic calcium deposits in gastric mucosa (A, HE, x100) verified with Voncossa stain (B, Von Cossa, x200).
Figure 2B: Amorphous basophilic calcium deposits in gastric mucosa (A, HE, x100) verified with Voncossa stain (B, Von Cossa, x200).
Discussion
Generally, gastric mucosal calcinosis (GMC) is only rarely encountered in routine biopsies. They have been associated with a wide spectrum of clinical conditions. The underlying mechanism by which a given cell or group of cells accumulate calcium is unclear. It has been suggested that calcium enters the cell by passive diffusion attributable to the concentration gradient across the gastric cell membrane, and that accumulation occurs when the ability to extrude these salts is exceeded. Gastric mucosal calcinosis (GMC) may be secondary to hypercalcemia, hyperphosphatemia, atrophic gastritis, hypervitaminosis A, chronic kidney disease, tumor lysis syndrome, organ transplantation, gastric neoplasia, or may be associated with use of citrate-containing blood products, aluminum-containing antacids, sucralfate or bismuth [1-6]. GMC may rarely cause symptoms such as epigastric pain or dyspepsia [7,8]. The clinical relevance of GMC remains to be seen. In theory, however, accelerated bone demineralization via loss of phosphates and absorption of aluminum in the gastrointestinal tract may be a consequence of long-term aluminum-containing antacid or sucralfate therapy. Furthermore, some examples of systemic calcification are reversible with normalization of biochemical parameters, which highlights the need for pathologists to highlight this finding when encountered in a premortem gastric biopsy. Our patient had no history of renal failure, organ transplantation, gastric malignancy or drug use.
Gastric mucosal calcinosis is categorized by some investigators into three subtypes as metastatic, dystrophic and idiopathic. Metastatic calcification is defined as the deposition of calcium salt in normal tissue due to an abnormal serum biochemical environment such as hypercalcaemia or hyperphosphataemia [1,2,7]. Metastatic calcification is the most common subtype and is seen in the presence of hypercalcemia, hyperphosphatemia or high levels of CaxPO4 products [9,15]. In cases with systemic calcification, gastric calcinosis improves when metabolic parameters improve. Dystrophic calcification develops in inflammatory, fibrotic and other pathological conditions. Metastatic calcification develops also in the kidneys, heart and liver. Our patient had no cancer, euthyroid lysis syndrome, antacid use or any of the other known risk factors. Our case was a very rare one and no etiology could be found for gastric mucosal calcinosis. The patient was recommended to return for endoscopic and clinic follow-up in 6 to 12-month intervals.
References
- Gorospe M, Fadare O. Gastric mucosal calcinosis: clinicopathologic considerations. Adv Anat Pathol. 2007; 14: 224-228. Ref: https://goo.gl/waQKkJ
- Avci Z, Alioglu B, Canan O, Ozcay F, Celasun B, et al. Calcification of the gastric mucosa associated with tumor lysis syndrome in a child with non-Hodgkin lymphoma. J Pediatr Hematol Oncol. 2006; 28: 307-310. Ref: https://goo.gl/bx4He1
- Seifert G. [Heterotopic (extraosseous) calcification (calcinosis). Etiology pathogenesis and clinical importance]. Pathologe. 1997; 18: 430-438. Ref: https://goo.gl/ncrSDr
- Saab S, Venkataramani A, Behling CA, Savides TJ. Gastric mucosal calcinosis in a patient with dyspepsia. J Clin Gastroenterol. 1996; 22: 156-164. Ref: https://goo.gl/tXkyDM
- Stroehlein KB, Stroehlein JR, Kahan BD, Gruber SA. Gastric mucosal calcinosis in renal transplant patients. Transplant Proc. 1999; 31: 2124-2126. Ref: https://goo.gl/EijRX5
- Greenson, Joel K, Trinidad, Salvador B, Pfeil, Sheryl A, et al. Gastric Mucosal Calcinosis: Calcified Aluminum Phosphate Deposits Secondary to Aluminum-Containing Antacids or Sucralfate Therapy in Organ Transplant Patients. American Journal of Surgical Pathology. 1993; 17: 45-50. Ref: https://goo.gl/Tbo1pU
- Yılmaz B, Köklü S, Sökmensüer C. Gastric mucosal calcinosis. Endoscopy. 2013; 45. Ref: https://goo.gl/XD7Qxk
- Kyoung Suk Lee, Su Ok Lee, Hyang Eun Seo, Jae Kwon Jung, Yoon Jin Jung, et al. Gastric Mucosal Calcinosis. The Korean Journal of Medicine. 2011; 81: 68-68. Ref: https://goo.gl/q8b92M
- Gorospe M, Fadare O. Gastric mucosal calcinosis-Clinicopathologic considerations. Advances in anatomic pathology. 2007; 14: 224-228. Ref: https://goo.gl/dZ4Ryx
- Nayak HK, Mohindra S, Iqbal S, Saraswat VA, Agarwal V, et al. Gastric Mucosal Calcinosis Mimicking Malignancy. The American Journal of Gastroenterology. 2016; 111: 1380. Ref: https://goo.gl/bDqStS
- Gray M, Brock A, Lodhia N. Gastric mucosal calcinosis: a rare cause of bleeding. Clin Gastroenterol Hepatol. 2014; 12: 22. Ref: https://goo.gl/B5rrBJ
- Hsieh TH, McCullough A, Agel B. Gastric mucosal calcinosis. Gastrointest Endosc. 2011; 73: 1282-1283. Ref: https://goo.gl/wAu9r4
- Matsukuma K, Gui D, Olson KA, Tejaswi S, Clayton EF, et al. OsmoPrep-associated Gastritis: A Histopathologic Mimic of Iron Pill Gastritis and Mucosal Calcinosis. Am J Surg Pathol. 2016; 40: 1550-1556. Ref: https://goo.gl/HBr7Vt
- Hiba MR, Eaker EY. The white plaque represents gastric mucosal metastatic calcification, which stains as dark deposits in the submucosa. Gastroenterology. 2000; 119: 894. Ref: https://goo.gl/gVCwfR
- Nakamura Y, Gotoh M, Fukuo Y, et al. Severe Calcification of Mucocutaneous and Gastrointestinal Tissues Induced by High Dose Administration of Vitamin D in a Puppy. J Vet Med Sci. 2004; 66: 1133-1135. Ref: https://goo.gl/DCSqP3