Case Report
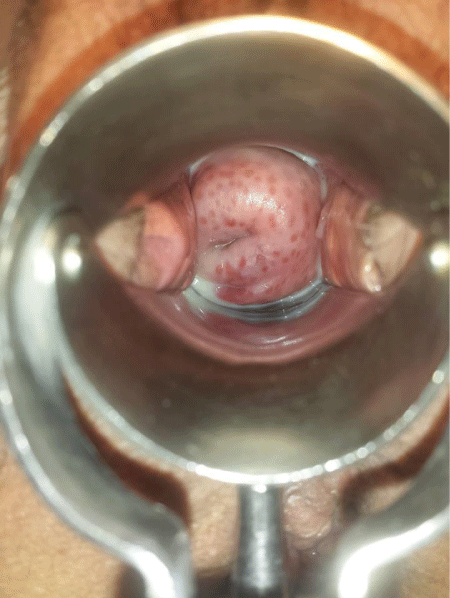
Trichomonas Vaginalis-A Clinical Image
Astrit M Gashi*
Department of Obstetrics and Gynecology, University Clinical Centre of Kosovo, Pristine, Kosova
*Address for Correspondence: Dr. Astrit M Gashi, Department of Obstetrics and Gynecology, University Clinical Centre of Kosovo, Pristine, Kosova, Email: [email protected]
Dates: Submitted: 28 June 2017; Approved: 20 July 2017; Published: 21 July 2017
How to cite this article: Gashi AM. Trichomonas Vaginalis-A Clinical Image. Arch Case Rep. 2017; 1: 001-002. DOI: 10.29328/journal.hjcr.1001001
Copyright License: © 2017 Gashi AM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A 32-year-old G4P301LC3 woman presents to the office for a visit, with a 6-day history of vaginal discharge with an unpleasant odor. On speculum examination, the discharge was green in color and frothy in appearance. Is noticed vulvar erythema, edema, and pruritus, also is noted the characteristic erythematous, punctate epithelial papillae or “strawberry” appearance of the cervix. Vaginal pH was 6.2. Diagnosis of Trichomonas vaginalis is made via wet prep microscopic examination of vaginal swabs.But also, for diagnosis help even the exam with the speculum, concretely “strawberry” appearance of the cervix. The diagnosis is confirmed by culture.Trichomoniasis is a sexually transmitted infection [1,2], that caused by trichomonas vaginalis. Trichomonas vaginalis is a unicellular, anaerobic flagellated protozoan, that inhabits the lower genitourinary tracts of women and men, but that can cause vaginitis. Clinical findings of Trichomonas vaginalis include a profuse discharge with an unpleasant odor. The discharge may be yellow, gray, or green in color and may be frothy in appearance. Vaginal pH is in the 6 to 7.Vulvar erythema, edema, and pruritus can also be noted. The characteristic erythematous, punctate epithelial papillae or “strawberry” appearance of the cervix is apparent in only 10% of cases. Symptoms are usually worse immediately after menses because of the transient increase in vaginal pH at that time. Diagnosis of Trichomonas vaginalis is made via wet prep microscopic examination of vaginal swabs. Other, more sensitive tests are available, including nucleic acid probe study and immunochromatographic capillary flow dipstick technology. The diagnosis can be confirmed when necessary with culture, which is the most sensitive and specific study. Nucleic acid amplification tests (NAATs) have replaced culture as the gold standard. T vaginalis NAATs have been validated in asymptomatic and symptomatic women and are a highly sensitive test [3]. Because the Trichomonas vaginalis is a sexually transmitted infection, both partners should be treated to prevent reinfection. The mainstay of treatment for Trichomonas vaginalis infections is metronidazole. Treatment schemes can be:
• Metronidazole 500 mg orally twice a day for 7 days, or 2 g orally in a single dose. OR
• Tinidazole 2 g orally in a single dose.
• If this treatment is unsuccessful, then Tinidazole or Metronidazole 2 g orally daily for 5 days is prescribed [4].
References
- Forna F, Gülmezoglu AM. Interventions for treating trichomoniasis in women. Cochrane Database Syst Rev. 2003. Ref.: https://goo.gl/rERNtp
- Van Der Pol B. Trichomonas vaginalis infection: the most prevalent nonviral sexually transmitted infection receives the least public health attention. Clinical Infectious Diseases. 2007; 44: 23-25. Ref.: https://goo.gl/CW3XLR
- American Journal of Obstetrics and Gynecology. 2004; 190: 281e90.
- Workowski KA, Berman S. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. MMWR Recomm Rep. 2006; 55: 1-94. Ref.: https://goo.gl/aNSeKN