More Information
Submitted: September 19, 2025 | Approved: October 31, 2025 | Published: November 03, 2025
How to cite this article: Sharma M, Chanchlani V, Kumari K, Vaishnav JK. A Case Series of Unexplained Somatic Symptoms of gilhari Syndrome - A Culture-bound Syndrome and Review. Arch Case Rep. 2025; 9(11): 342-345. Available from:
https://dx.doi.org/10.29328/journal.acr.1001171
DOI: 10.29328/journal.acr.1001171
Copyright license: © 2025 Sharma M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Otorhinolaryngology; Psychiatry otorhinolaryngology; Psychiatry; Culture-Bound Syndromes (CBS); Dhat syndrome; gilhari syndrome; Somatic symptoms
A Case Series of Unexplained Somatic Symptoms of gilhari Syndrome - A Culture-bound Syndrome and Review
Mini Sharma1*, Veerbhan Chanchlani2, Kanchan Kumari3 and Jairaj Kumar Vaishnav4
1Assistant Professor, Department of Psychiatry, RVRS Government Medical College, Bhilwara, Rajasthan, India
2Professor & Head, Department of Psychiatry, RVRS Government Medical College, Bhilwara, Rajasthan, India
3Senior Resident, Department of Psychiatry, JNU Medical College, Jaipur, Rajasthan, India
4Associate Professor, Department of Otorhinolaryngology, RVRS Government Medical College, Bhilwara, Rajasthan, India
*Address for Correspondence: Dr Mini Sharma, Assistant Professor, Department of Psychiatry, RVRS Government Medical College, Bhilwara, Rajasthan, India, Email: [email protected]
Culture plays an important role in shaping the emotional & behavioral expression of a person. Many times, our beliefs color the psychological and somatic symptoms of psychiatric illness as seen in various culture-bound syndromes. We are describing 3 cases of one such culture-bound syndrome called gilhari syndrome. In the management of these cases, special consideration to phenomenology is needed along with consultation and liaison with various specialties.
Culture-bound syndromes (CBS) are psychological and somatic symptoms recognized within specific cultures or societies but not easily classified in standardized psychiatric categories like DSM-5 or ICD-11 [1,2]. Among the various known CBS like Dhat syndrome, Koro syndrome, Possession syndrome, etc., gilhari (lizard) syndrome was studied especially in the Rajasthan region. In gilhari (Lizard) syndrome, people believe that the gilhari rises in the back and later reaches the neck of the person, which will kill him/her. This reliance is so strong that the patient and their careers follow rituals to crush this crawling gilhari & feel relieved. Because of the presence of various somatic features influenced by cultural beliefs, it’s often difficult to diagnose CBS. Individuals with these physically distressing symptoms experience a significant dysfunction in social & occupational functioning, affecting their quality of life. The pathway to care among these is extended from faith healers to quacks to physicians & other specialists and eventually to mental health-care professionals. This late addressed issue is attributable to a lack of knowledge and acknowledgment of the symptoms due to gilhari syndrome, which causes a significant delay in seeking mental health professional help due to various faith healing practices & other specialty consultations [3].
Case report 1
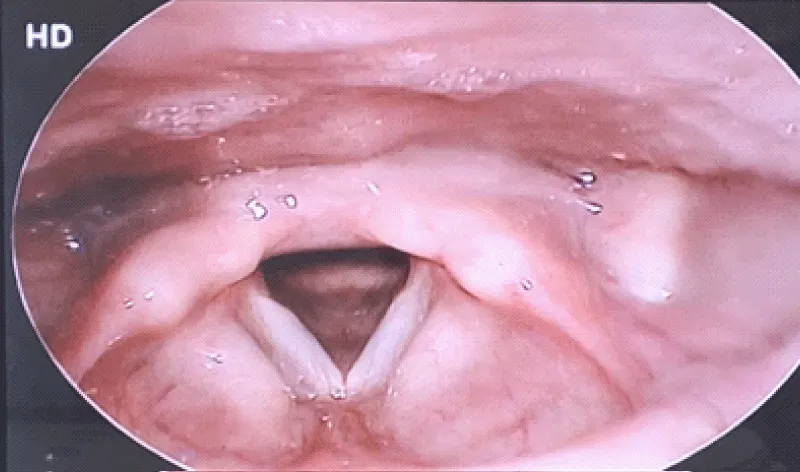
A twenty-four-year-old married female presented to the Otorhinolaryngology outpatient department with complaints of progressive dysphagia over the past 2 years. She initially felt a feeling of solid food stuck in her throat, which over the next year progressed to difficulty swallowing solid food. The patient would now consume a semi-solid and liquid diet only. Over 8-9 months, she would also feel difficulty in drinking liquids, due to some choking sensations in her throat. The patient would report to her mother that a globular mass is pressing her throat, and it would choke her to death. The patient was provisionally diagnosed with Globus Dysphagia, and symptomatic treatment was advised. She was further evaluated for the etiology of her symptoms. Patient’s physical and detailed oral-pharyngeal examinations (Figure 1) were found to be normal. Her laryngoscopy and endoscopy evaluation revealed a totally normal anatomy and functioning.
Figure 1: Laryngoscopy showing vocal cords and adjacent region.
Apart from these complaints, she would also experience some vague bodily problems in the form of a crawling sensation in her legs and back, ghabrahat (colloquial expressions of subjective anxiety), restlessness, and weakness. Considering the same, a psychiatric opinion was planned for the patient. On evaluation, the patient reported that she was experiencing a sensation of a small organism crawling over her body. She called it “Jeev chalta hai sharir mein” (meaning: an organism keeps crawling on her body). Further, she explained that over the past 4 years, this jeev has gradually ascended from her lower limbs to her back, and now it’s stuck in her neck region. It’s probably because of this organism that she has been experiencing pressure & difficulty swallowing, along with anxiety, over the past 2 years.
The patient was started on a capsule of fluoxetine 20 mg per day, titrated up to 40 mg per day along with a tablet. Olanzapine 5 mg per day & tab. Clonazepam 0.5 mg per day. Patient responded well over 8 weeks and continued follow-up over the next 6 months with full remission.
Case report 2
A 28-year-old unmarried laborer presented with complaints of ghabrahat (colloquial expressions of subjective anxiety), restlessness, feeling of impending doom & scratching of the back over the past 10 months. On examination, there were marks of skin excoriations and some small linear scar marks over his back, while his rest physical examination was normal. The patient was evaluated for possible metabolic and endocrine causes, which were found to be normal. He was started on the tab. Propranolol 40 mg per day in and tablet. Clonazepam 0.5mg per day for the diagnosis of Anxiety nos.
The patient was also consulted with the Dermatologist to evaluate for the excoriation. No dermatological condition was found; rather, it was reported that due to some sensations patient would scratch his back. On further assessment, he reported that he would feel a small, round mass that was drifting from one side to another over his back, because of which he would scratch his back. He further on evaluation reported that it is a small animal that has entered his body from the back & is now moving around his back. He also reported similar incidents that his grandparents had narrated to him about their village, where people would possess this animal and would even choke & suffocate. Because of this believed he would experience severe anxiety whenever he would experience the movement over his back.
The patient was then started on capsule fluoxetine to a maximum dose of 60 mg/day along with 1mg of tab. Risperidone per day. Patient showed up to 75% response at 2 months of treatment. Later, he would often be irregular in follow-up and visit faith healers where his back would be incised so that the animal would come out of his body. This further exacerbates his symptoms. He, along with his family members, was psycho-educated about the illness and treatment needs, but due to strong cultural beliefs, they would continue to follow faith healing rituals along with irregular medications.
Case report 3
A 19years adolescent came to the Otorhinolaryngology outpatient department holding neck with complaints of swelling and pain over the past 1 year. As per her, this swelling would appear on either side of the neck associated with pain-like sensation and episodes of ghabrahat (colloquial expressions of subjective anxiety) or hyperventilation lasting from 1-2 hours and would subside when this swelling reduced. There was no history of fever, dysphagia, weight loss, easy fatigability, or any signs of local tenderness & palpable mass. The patient was thoroughly evaluated for underlying pathology by laryngoscopy, endoscopy, neck x-ray, and ultrasonography, which also showed a normal study. Despite symptomatic management, there was no relief, and hence, a consultation liaison with the Psychiatry department was taken.
On mental status examination patient showed distress about the swelling rising in her neck and sensation of something moving in her body. She would feel pressure associated with pain when this mass would move up towards the surface and over the neck region. She also reported her belief that it’s a small animal that shifts around and causes these symptoms. The patient was started on tab. Escitalopram 10 mg was built up to 2 mg / gay, and Risperidone 1mg per day over 9 weeks, during which response was seen.
All the above-stated cases belonged to the southern part of Rajasthan. All were young in the second & third decades of life, among whom the majority were female. They had a similar belief that a small animal/ organism moving over their body led to somatic symptoms. These syndromes reflect the influence of cultural beliefs, environmental stressors, and social frameworks on mental health presentations. In the Indian context, several CBS have been identified and documented in psychiatric literature, including Dhat syndrome, Koro, Possession states, Bhut-vidya phenomena, and the relatively localized gilhari syndrome. India’s culturally diverse population provides fertile ground for unique syndromes to emerge, shaped by regional beliefs and idioms of distress. For example, Dhat syndrome, prevalent in North India, is characterized by anxiety and fatigue attributed to semen loss [3]. Similarly, Possession syndromes are interpreted as spirit intrusions in several rural communities. These syndromes often overlap with somatoform, anxiety, or depressive disorders and require a culturally informed diagnostic and therapeutic approach [4].
Epidemiology of culture-bound syndromes: Global and indian perspectives
Culture-bound syndromes have been identified across continents, particularly in Asia, Africa, and Latin America, where indigenous cultural practices and belief systems strongly influence expressions of mental distress [5]. While many of these conditions do not align with Western psychiatric diagnostic frameworks, they are deeply rooted in the socio-cultural fabric of the communities they arise from [6] (Table 1).
| Table 1: Some well-documented CBS worldwide include. | ||
| Culture Bound Syndrome | Region | Symptoms |
| Koro | South-East Asia | Intense fear of genital retraction and death. |
| Amok | Malaysia, Indonesia | Sudden, unprovoked violent outbursts |
| Ataque de nervios | Latin America | Acute episodes of intense emotional upset |
| Hwabyeong | Korea | Anger-related somatic syndrome |
| Susto | Latin America | Illness due to sudden fright or soul loss |
The prevalence of CBS varies widely depending on region, culture, and the variability of disorder symptoms. A WHO study (1993) on somatoform disorders found that up to 20% - 30% of primary care patients in non-Western countries may present with culture-specific syndromes. In China and Southeast Asia, ‘Koro epidemics’ have been reported multiple times, particularly in the 20th century. Even in India, with its complex social structure and rich traditions, it has contributed several case studies to psychiatric literature. The most studied include:
1. Dhat syndrome: A syndrome where semen loss is associated with anxiety and other vague bodily complaints. Its estimates vary from 12% to 30% among young males attending general and psychiatric outpatient clinics in northern India [7]. It is more prevalent in lower socio-economic groups, especially in North India and Nepal.
2. Possession syndromes: A syndrome that presents as dissociative trance or possession states, commonly among tribal and rural areas. Its prevalence varies from 3% to 15% in psychiatry clinics, particularly among women and adolescents [8].
3. Koro (in Eastern India and Northeast India): Though typically associated with Southeast Asia, several Koro epidemics have been reported in West Bengal and Assam, where a person comes with a strong belief that their genitalia will shrink and disappear. A study in Kolkata during an epidemic in 2010 showed a sharp rise in psychiatric emergency visits among young males [9-11). Yap portrayed Koro patients as dependent, immature, and lacking confidence in their virility and being in steady sexual conflicts [12].
4. gilhari syndrome (Rajasthan): No formal epidemiological study exists, but regional reports suggest clusters among school-age and adolescent populations. Anecdotal reports suggest up to 10–15 cases per month are reported in the Bikaner region of Rajasthan.
gilhari syndrome: A regional culture-bound syndrome from Rajasthan
gilhari Syndrome (‘lizard’ or ‘squirrel syndrome’) has been documented in the Bikaner region of Rajasthan, primarily among adolescents and young adults. The condition is characterized by patients reporting a sensation of a small animal—most commonly described as a squirrel—moving up and down the spine. This perception is not associated with any identifiable neurological or dermatological condition but causes considerable distress and functional impairment [6,13-15].
Although not officially classified in international diagnostic systems, gilhari syndrome has been acknowledged in regional psychiatric case studies and conference reports. According to a study conducted at SP Medical College, Bikaner, this syndrome is reported to appear as psychosomatic in origin and is often linked with academic pressure, social stress, and low mental health literacy [5]. The syndrome is commonly seen in individuals who may somatize psychological distress due to the stigma of mental illness or lack of emotional vocabulary.
gilhari Syndrome has core features of sudden onset of behavioral disturbances, often dramatic and bizarre, that include: shouting, crying, fainting spells, refusal to eat, agitation, or unusual movements. Another marked feature is that it’s often perceived to be due to some supernatural force, such as evil spirits, black magic, or possession. The syndrome is mostly seen in young women or adolescent girls, especially in socially stressful contexts.
Treatment approaches include psycho-education, reassurance, supportive psychotherapy, and, in some cases, cognitive-behavioral therapy. In pharmacological intervention, anxiolytics or antidepressants are reported to be beneficial. However, cultural misconceptions often lead patients to seek faith healers or traditional remedies before reaching psychiatric care [3,6].
Other major challenges in the management of CBS include unreported symptoms due to stigma, cultural normalization, or patients seeking traditional rather than psychiatric care. Another issue is the lack of large studies with a clear formulation for evaluation and guidelines for the management of CBS. Our current available literature is limited to various epidemiological studies, like case series, hospital-based data, or qualitative reports, etc [9].
Culture-bound syndromes are an important shade in the psychiatric disorder spectrum. gilhari syndrome is endogenously prevalent in Rajasthan and often under- or misdiagnosed due to the presence of various somatic symptoms. Another important issue for a huge treatment gap is seeking a cure by various traditional practices & faith healing methods, which further deteriorate the illness and impact the quality of living of patients. Hence, an awareness about the CBS, a holistic approach to evaluation and management, and a large studies about CBS would be beneficial for understanding CBS.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington (DC): American Psychiatric Association; 2013. Available from: https://psycnet.apa.org/record/2013-14907-000
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1993. Available from: https://www.who.int/publications/i/item/9241544228
- Grover S, Gupta S, Avasthi A. Dhat syndrome: A review. Indian J Psychol Med. 2015;37(2):129–137.
- Isaac M. Culture and Common Mental Disorders in India. Oxford: Oxford University Press; 2001.
- Akhtar S. Four culture-bound psychiatric syndromes in India. Int J Soc Psychiatry. 1988;34:70–74. Available from: https://doi.org/10.1177/002076408803400109
- Jain A, Kamal Kumar V, Omprakash J, Suthar N. “gilhari (Lizard) Syndrome” – A new culture-bound syndrome. J Psychiatry. 2014;17:117. Available from: https://doi.org/10.4172/1994-8220.1000117
- Behere PB, Natraj GS. Dhat syndrome: The phenomenology of a culture-bound sex neurosis of the Orient. Indian J Psychiatry. 1984;26(1):76–8. Available from: https://pubmed.ncbi.nlm.nih.gov/21965960/
- Chaturvedi SK, Broota A. Possession syndrome in North India. Indian J Psychiatry. 1989;31(3):235–242.
- Kar SK, Chandrima RM. Koro epidemics in India: Review of the literature and case reports. J Indian Assoc Child Adolesc Ment Health. 2011;7(2):60–66.
- Durst R, Rosca-Rebaudengo P. The disorder named Koro. Behav Neurol. 1991;4(1):1–13. Available from: https://doi.org/10.3233/ben-1991-4101
- Edwards JW. Indigenous Koro, a genital retraction syndrome of insular Southeast Asia: A critical review. Cult Med Psychiatry. 1984;8(1):1–24. Available from: https://doi.org/10.1007/bf00053099
- Yap PM. Classification of the culture-bound reactive syndromes. Aust N Z J Psychiatry. 1967;1:172–9. Available from: https://doi.org/10.3109/00048676709159191
- Littlewood R, Lipsedge M. Aliens and Alienists: Ethnic Minorities and Psychiatry. Harmondsworth: Penguin Books; 1985. Available from: http://ndl.ethernet.edu.et/bitstream/123456789/3025/1/91.pdf
- Ventriglio A, Ayonrinde O, Bhugra D. Relevance of culture-bound syndromes in the 21st century. Psychiatry Clin Neurosci. 2016;70(1):3–6. Available from: https://doi.org/10.1111/pcn.12359
- Verma K, Bhojak M, Singhal A, Jhirwal O, Khunteta A. “Gilahari (Lizard) Syndrome”: Is it a new culture-bound syndrome? A case report. Indian J Psychiatry. 2001;43(1):70–72. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2955937/