More Information
Submitted: August 12, 2025 | Approved: August 25, 2025 | Published: August 26, 2025
How to cite this article: Polat E, Kocoglu H, Solcan SI. Combination of Interscalen Brachial Plexus Block and Superficial Cervical Plexus Block in The Patient to be Operated on for Clavicular Excision of Chordoma: A Case Report. Arch Case Rep. 2025; 9(8): 269-272. Available from:
https://dx.doi.org/10.29328/journal.acr.1001158
DOI: 10.29328/journal.acr.1001158
Copyright license: © 2025 Polat E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Cervical plexus block; Brachial plexus block; Clavicle surgery
Combination of Interscalen Brachial Plexus Block and Superficial Cervical Plexus Block in The Patient to be Operated on for Clavicular Excision of Chordoma: A Case Report
Ezgi Polat1*, Hasan Kocoglu2 and Seyit Ibrahim Solcan2
1Department of Anesthesiology and Reanimation, Medipol Acibadem Regional Hospital, Istanbul, Turkey
2Department of Anesthesiology and Reanimation, Faculty of Medicine, Istanbul Medeniyet University, Istanbul, Turkey
*Address for Correspondence: Ezgi Polat, Department of Anesthesiology and Reanimation, Medipol Acibadem Regional Hospital, Istanbul, Turkey, Email: [email protected]
Background: Clavicular surgery can be performed under general or regional anesthesia with peripheral nerve blocks.
Case: A 29-year-old man with cerebrovascular disease, interstitial lung disease, a tumour in the lung, right vocal cord paralysis, cervical, thoracic, and lumbar stabilization was scheduled for regional anesthesia to undergo metastatic chordoma at the clavicle. Considering the risks, the patient who will be operated on for tumour excision in the right clavicle, who is predicted to have difficult intubation due to limitation of extension secondary to a previous posterior cervical instrumentation, is treated with interscalene brachial plexus block and superficial cervical plexus block combination to avoid multiple drug use and complications that may arise during intubation.
Conclusion: Regional anesthesia seems like a reasonable alternative to general anesthesia and may be a good option for perioperative analgesia management in clavicle surgery.
Chordoma is a rare primary bone cancer that mainly affects the skull base, spine, and sacrum [1]. Although chordomas grow slowly and are localized, they often have the characteristics of being locally aggressive and causing chronic pain [2]. Even after surgery and/or radiation, chordomas can recur and lead to multiple surgeries within a few years. Tumor metastases to the lungs, liver, bones, and skin occur in 20% - 40% of patients with spinal chordoma [3]. The main indication for interscalene brachial plexus block (ISBPB) is suprascapular, lateral pectoral, axillary nerve, and shoulder surgeries that indicate C4 blockade [4]. Studies are showing that superficial cervical plexus block (SCPB) is mostly used in neck surgeries such as carotid endarterectomy and thyroid surgery, as well as in clavicle surgery [5-7]. Sensory innervation of the clavicle is controversial, so although regional anesthesia applications are limited, studies are showing that combined brachial plexus block and superficial cervical plexus peripheral nerve block ensure effective anesthesia for clavicle surgical procedures [7,8].
In this case, a patient in whom we applied an interscalene block and superficial cervical plexus block using bupivacaine and lidocaine with Ultrasound (US), stimplex is presented.
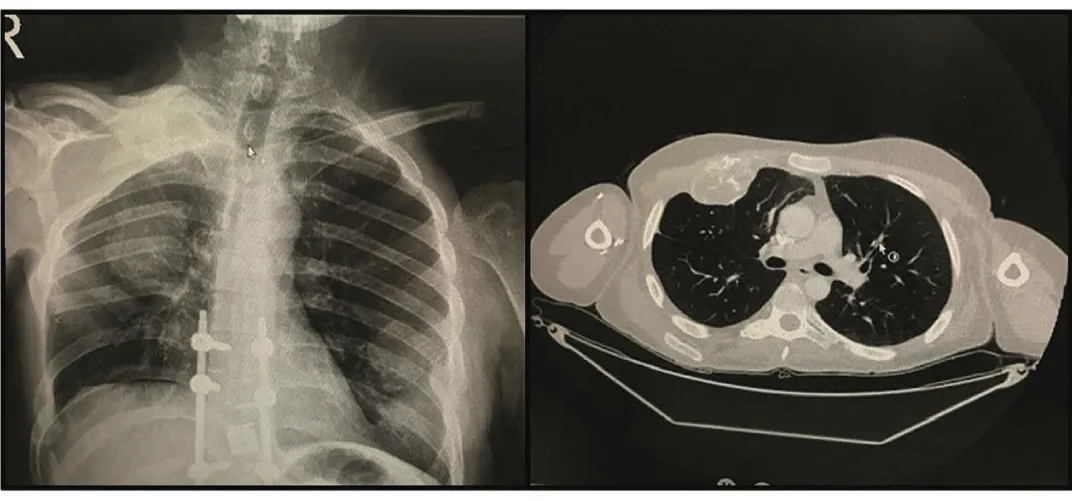
Recurrent metastatic chordoma was detected in the patient who applied to Istanbul Medeniyet University Orthopedics and Traumatology Clinic because of a fixed, hard tumour under the skin in the right clavicle. The patient was 29 years old, 180 cm in height, 73 kg in weight, and ASA IV. In his background, he had a previous history of cerebrovascular disease (cured without sequelae, no neurological deficit), interstitial lung disease, right lung tumour, right vocal cord paralysis, cervical, thoracic, and lumbar stabilization operations due to chordoma (Figure 1).
Figure 1: X-ray and tomography image of the patient.
In the physical examination, severe limitation of head and neck movements was detected, and the Mallampati score was II. Lung sounds were decreased in the right apex, and no additional sound was heard. In the flexible laryngoscopic examination performed by an ear, nose, and throat specialist, it was reported that the right vocal cord was paralytic and the right arytenoid was edematous, and the left vocal cord was normal.
In the evaluation made by a pulmonologist, it was determined that FVC (forced vital capacity): 44%, FEV1(Forced Expiratory Volume in one Second): 47%, FEV1/FVC: 109% in pulmonary function tests, was consistent with severe restriction. The patient with partial loss of aeration, pleural thickening, parenchymal recessions, fibrotic changes, and bronchiolitis, in addition to mass formation in the right lung, was evaluated as high risk in the thorax tomography. The patient, whose consent was obtained, was taken to the operating room without premedication. ISBPB and SCPB were planned to be performed instead of general anesthesia due to the presence of difficult intubation criteria and the avoidance of respiratory complications in the patient, who was evaluated as high risk by a pulmonologist. The patient was taken to the operating room, and isotonic infusion was started after the vascular access was established from the dorsal side of the left hand with a 20-G intravenous cannula. The patient was monitored by electrocardiography, noninvasive Blood Pressure (BP), Heart Rate (HR), and peripheral oxygen saturation (SpO2) values. Vitals BP: 126/65 mmHg HR: 93 beats (rhythmic) SpO2: 93%. Four lt. min-1 oxygen insufflation was provided with the mask. Informed the patient about the procedure. For sedoalgesia, 1 mg of Dormicum and 25 μg of fentanyl were administered. The head could not be turned to the opposite side of the side where the block was to be made; there was also a limitation of rotation as well as a limitation of extension. The right side of the neck was disinfected with povidone iodine and covered with a sterile compress. The anode (+) end of the nerve stimulator (Plexygon Nerve Stimulator, VYGON, 7501 31) was connected to the ECG electrode placed distal to the right hand. A fifty mm long (Echo plex+, 20 O, VYGON, Ecouen, FRANCE) 21 G peripheral block needle was connected to the cathode (-) pole of the stimulator. The US (Samsung Ultrasound, MODEL: SW2F-45EB) high-frequency linear probe was prepared sterilely. The interscalene brachial plexus was visualized by US. Then, at this point, following the application of subcutaneous local anesthesia to the skin, the stimulator needle was advanced to the probe between the anterior and middle scalene muscles with a long-axis approach (in-plane), and the nerve stimulator was opened up to 1 mA after the skin was penetrated through the subcutaneous tissue.
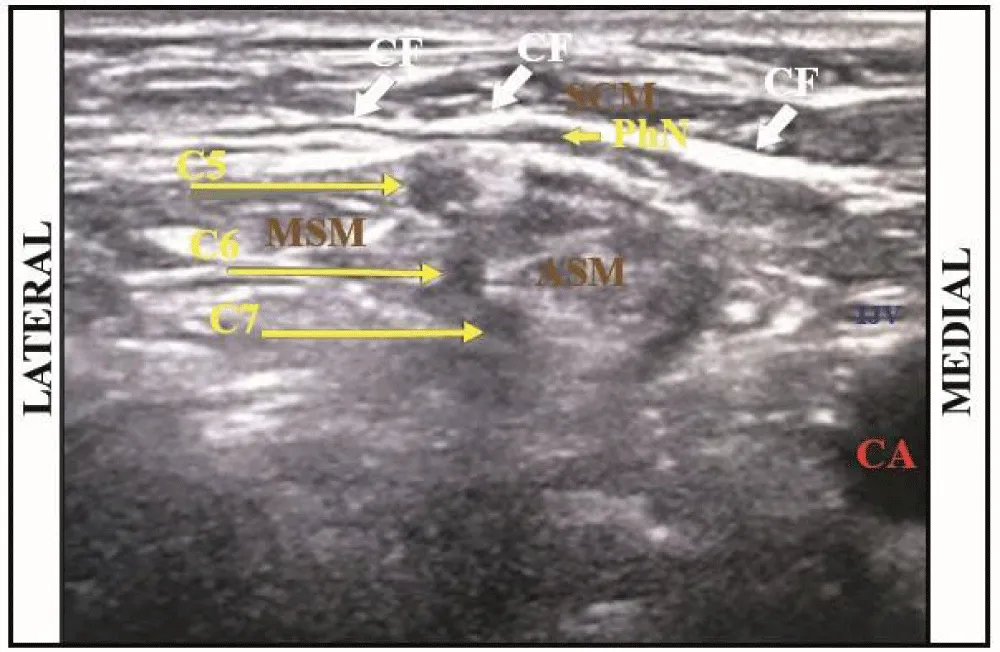
Following motor movement in the shoulder, the stimulator is reduced to 0. 3-0. 5 mA and motor movements are observed for 0. 1 ms, while negative aspiration is followed by 10 ml of 0. 5% bupivacaine (Buvacin 0. 5% vial, Vem İlaç Sanayi ve Ticaret Ltd. Sti., Istanbul -Turkey) + 5 ml 2% lidocaine (2% Lidocaine ampoule, Polifarma İlaç Sanayi ve Ticaret Ltd. Sti., Tekirdag -Turkey) was applied. SCPB was applied with 10 ml of 0. 5% bupivacaine and 5 ml of 2% lidocaine with the in-plane technique. Superficial cervical block and interscalene block were applied to the patient in the chaise longue position. Adequate sensory and motor block was ensured for the patient, and the operation was completed without complications (Figure 2).
Figure 2: Ultrasound image. CA: Carotis Arter; IJV: Internal Jugular Vein; SCM: Sternocleidomastoid Muscle; ASM: Anterior Scalene Muscle; MSM: Middle Scalene Muscle; PhN: Phrenic Nerve; CF: Cervical Fascia
Thus, a 29-year-old male patient was prepared for surgery for chordoma excision from the right clavicle. The operation was started after 20 minutes. The patient was sedated with 1 mg Dormicum + 25 mg ketamine at 45-minute intervals throughout the operation.
Ramsey Sedation Scale was evaluated as 3 throughout the operation. The operation lasted for 120 minutes. The mass (7 cm) was excised from the lateral clavicle without any complications, and cement was applied to the right clavicle (Figure 3).
Figure 3: Peroperative surgical process.
Regional anesthesia has a strong role in minimizing postoperative pain, reducing narcotic use, postoperative nausea/vomiting, and shortening the time of discharge [9]. Peripheral nerve blocks have begun to take place in daily practice, especially due to the development of technology and clinical understanding of anatomical sonography in recent years. Recent research has shown that direct visualization of the distribution of local anesthetics with high-frequency probes can improve block quality and prevent complications from upper/lower extremity nerve blocks and neuraxial techniques [10].
Although the information about clavicle surgery under regional anesthesia is limited in the literature, there are various studies.
Hering, et al. [11] applied a superficial cervical plexus block with 8 ml of 0. 5% bupivacaine under US guidance to reduce the pain of a patient who presented to the emergency department with the complaint of severe pain in the clavicle after a fall. The patient’s pain score decreased from 9/10 to 2/10, and it was observed that the analgesic effect lasted for about 20 hours. A superficial cervical plexus block may be effective for postoperative analgesic effect, but not sufficient for intraoperative analgesia. For adequate intraoperative analgesia, an interscalene or supraclavicular brachial plexus block and support block are required in most cases. Baran, et al. [7] performed a superficial cervical plexus block and a supraclavicular brachial plexus block with combined 5 ml 5% bupivacaine and 5 ml 2% lidocaine by US-guided in a 38-year-old male patient who presented with a clavicle fracture. Complications and need for additional sedation had not developed. Reverdy [12] provided adequate anesthesia for clavicle surgery with a combined superficial cervical plexus block and supraclavicular brachial plexus block without general anesthesia in a pilot study conducted involving 12 patients in 2015. Rescue analgesia was not needed, and the patients had with mean VAS (visual analogue scale) score of 2 on postoperative day 0. And 1. The median for satisfaction was rated 8 on the simple numerical scale (This indicates great satisfaction with the anesthesia strategy). The patients were discharged on the postoperative day without any complications. Ryan, et al. [13] conducted a retrospective study of 110 patients, 52 of whom received regional anesthesia only with a combined block and 58 of whom received general anesthesia with an interscalene brachial plexus block. No major anesthesia-related complication was observed in any patient, and there was no case in which regional anesthesia had to be converted to general anesthesia due to block failure. Operations carried out with regional anesthesia took an average of 131 minutes. In the study, patients in the general anesthesia group required significantly more intraoperative fentanyl (207 μg vs. 141 μg, p = 002). At the same time, anesthesia initiation time (29 vs. 20 minutes, p = 022) was found to be significantly longer in the general anesthesia group.
As seen in our study in parallel with the literature, regional anesthesia applied with a combination of brachial plexus and superficial cervical plexus block is a safe and effective technique in clavicle surgery. Combined block seems like a reasonable alternative to general anesthesia to avoid multiple drug use and complications that may arise during intubation, and may be a good option for perioperative analgesia management.
- McMaster ML, Goldstein AM, Bromley CM, Ishibe N, Parry DM. Chordoma: incidence and survival patterns in the United States, 1973–1995. Cancer Causes Control. 2001;12:1–11. Available from: https://doi.org/10.1023/a:1008947301735
- McCain MA. Chordoma in a chronic pain patient. Arch Phys Med Rehabil. 1985;66(7):457–8. Available from: https://pubmed.ncbi.nlm.nih.gov/3160321/
- Catton C, O'Sullivan B, Bell R, Laperriere N, Cummings B, Fornasier V, et al. Chordoma: long-term follow-up after radical photon irradiation. Radiother Oncol. 1996;41(1):67–72. Available from: https://doi.org/10.1016/s0167-8140(96)91805-8
- Feigl GC, Litz RJ, Marhofer P. Anatomy of the brachial plexus and its implications for daily clinical practice: regional anesthesia is applied anatomy. Reg Anesth Pain Med. 2020;45(8):620–7. Available from: https://doi.org/10.1136/rapm-2020-101435
- Aunac S, Carlier M, Singelyn F, De Kock M. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg. 2002;95(3):746–50. Available from: https://doi.org/10.1097/00000539-200209000-00039
- Pandit JJ, Satya-Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. 2007;99(2):159–69. Available from: https://doi.org/10.1093/bja/aem160
- Baran O, Kır B, Ateş İ, Şahin A, Üztürk A. Combined supraclavicular and superficial cervical plexus block for clavicle surgery. Korean J Anesthesiol. 2020;73(1):67–70. Available from: https://doi.org/10.4097/kja.d.18.00296
- Fugelli CG, Westlye ET, Ersdal MD, Strand KD, Bjørshol C. Combined interscalene brachial plexus and superficial cervical plexus nerve block for midshaft clavicle surgery: a case series. AANA J. 2019;87(5):374–8. Available from: https://pubmed.ncbi.nlm.nih.gov/31612842/
- Shams D, Sachse K, Statzer N, Gupta RK. Regional anesthesia complications and contraindications. Clin Sports Med. 2022;41(2):329–43. Available from: https://doi.org/10.1016/j.csm.2021.11.006
- Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth. 2005;94(1):7–17. Available from: https://doi.org/10.1093/bja/aei002
- Herring AA, Stone MB, Frenkel O, Chipman A, Nagdev AD. The ultrasound-guided superficial cervical plexus block for anesthesia and analgesia in emergency care settings. Am J Emerg Med. 2012;30(7):1263–7. Available from: https://doi.org/10.1016/j.ajem.2011.06.023
- Reverdy F. Combined interscalene-superficial cervical plexus block for clavicle surgery: an easy technique to avoid general anesthesia. Br J Anaesth. 2015;115:eLetters Supplement. Available from: https://doi.org/10.1093/bja/el_12970
- Ryan DJ, Iofin N, Furgiuele D, Johnson J, Egol K. Regional anesthesia for clavicle fracture surgery is safe and effective. J Shoulder Elbow Surg. 2021;30(7):e356–60. Available from: https://doi.org/10.1016/j.jse.2020.10.009